- Basic information
- Center for comprehensive care for children with developmental disorders and their families
- Center for Diagnosis and Treatment of Ciliary Epithelial Disorders (Primary Ciliary Dyskinesia)
- Center for highly specialized care for rare liver diseases
- About the clinic
- History of the XNUMXst Children's Clinic
- History and present of the nephrology department of the Pediatric Clinic
- Sponsors
- Information for sponsors
- Gallery
- Doctors
- Working groups
- Nephrology and dialysis
- Pediatric pneumology
- Endocrinology
- Gastroenterology and nutrition
- List of physicians and contacts
- Information for patients
- Hypertension
- Monogenic diabetes in children
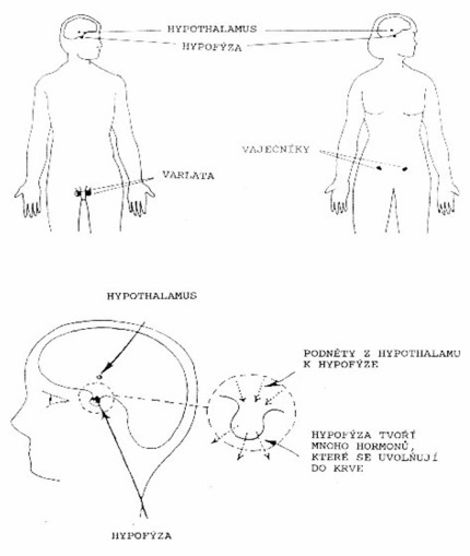
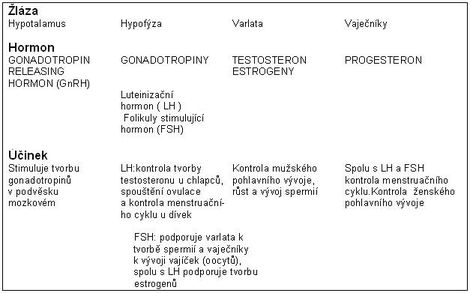
- The growth and maturation of the child
- Growth hormone treatment
- Turner syndrome
- For diabetics
- Premature adolescence
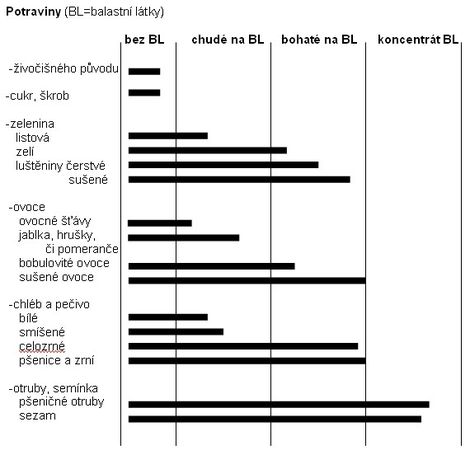
- Constipation
- Kidney disorders and transplantation
- Polycystic kidney disease
- For the professional public
- Seminars
- Research
- Science
- Specialization
- Contact
- Where to find us
- Examination orders
Basic information
 Dear friends, colleagues, co-workers and sponsors, pediatric patients and their parents!
Dear friends, colleagues, co-workers and sponsors, pediatric patients and their parents!
The Department of Pediatrics of the 2nd Faculty of Medicine of Charles University and the University Hospital in Motol was established in 2004 by merging the work teams of the former I. children's clinic and a significant part of the former II. children's clinic. It is a continuation of their mission - to provide highly specialized and erudite care to children from all over the Czech Republic, whose doctors or parents have requested it. The team of the Pediatric Clinic creates a natural professional background, the "ultimum refugium", for all Czech and Moravian pediatricians, whether they work in children's clinics of teaching hospitals, district children's wards or work as general practitioners for children and adolescents. We are ready to help you and your patients whenever you deem it necessary.
You also meet the staff of the Pediatric Clinic in undergraduate and postgraduate education in pediatrics and its subspecializations, in organizational activities in the care of sick children at the national level and in clinical research and development of biomedical knowledge for the benefit of pediatric patients.
In almost all areas of pediatrics and adolescent medicine, the Pediatric Clinic has highly qualified specialists who provide top diagnostics and therapy - in pediatric nephrology, dialysis and elimination methods, pediatric pneumology, allergology and care for children with cystic fibrosis, pediatric endocrinology and diabetology. , in pediatric gastroenterology and in the care of children with autoimmune diseases. In cooperation with partner workplaces of the Motol University Hospital, we also provide cardiological, immunological and hematological care.
The credo of the Pediatric Clinic team is "partnership for the benefit of pediatric patients". We are here for you and your patients. Our strength lies in the team experience, in the quality equipment and in the cooperation of the pediatric think tank of the Motol hospital. We strive for straightforward, fast and effective diagnosis and therapy with maximum care for our common pediatric patients.
Our work would be more difficult without sponsors, who make a significant contribution to the renewal and expansion of the clinic's equipment, our "instruments", but also to a friendly and aesthetic environment for our patients. Many thanks to all our sponsors, the clinic team and our patients.
Thanks also go to all Czech and Moravian pediatricians in primary care and inpatient facilities. We highly value their daily endless efforts. It is thanks to them and their work that the sick children who need it most come to us. We thank them for recommending and sending these patients to us. I am sure that it is through our joint efforts that we achieve the maximum possible for the well-being of sick children.
Prof. MUDr. Jan Lebl, CSc., On behalf of the team of doctors and nurses of the Pediatric Clinic
The head
Prof. MUDr. Zdenek Sumnik, Ph.D.
Primary
doc. MD Štěpánka Průhová, Ph.D.
224 432 003
pediatrie@fnmotol.cz
Other contacts
Medical Secretariat
224 432 002
jana.saskova@fnmotol.cz
224 432 004
lenka.viktorinova@fnmotol.cz
School secretariat
224 432 001
klara.borecka@fnmotol.cz
Contact with health insurance companies
224 432 007
jitka.doubravova@fnmotol.cz
Center for comprehensive care for children with developmental disorders and their families
Viz Center for comprehensive care for children with developmental disorders and their families
Center for Diagnosis and Treatment of Ciliary Epithelial Disorders (Primary Ciliary Dyskinesia)
The Center for Ciliary Epithelial Disorders at the University Hospital in Motol is the main workplace in the Czech Republic providing diagnosis and treatment for patients with this congenital disorder.
The Motol Center has been dealing with this topic for many years, in the last few years the center's equipment has been significantly improved and diagnostic methods and treatment procedures have been introduced in the form usual in most developed countries. It was also possible to significantly increase the detection of patients with this disorder, which allows for the timely introduction of medical care and thus improve the prognosis. Primary ciliary dyskinesia (PCD) is a rare disease, its incidence in our country is expected to be similar to that of cystic fibrosis, ie about 600 individuals. However, we still lack to detect about 500 patients with this number. They may be hiding under other diagnoses and thus do not receive proper comprehensive care. Their disease then unnecessarily causes them a number of significant problems and unnecessarily damages the lung tissue. We are therefore trying to raise awareness of this disease both among the general public and among health professionals.
Detailed information about our center and the disease can be found on the website www.rasinky.cz
Our workplace is a full member of the European Reference Network (ERN-LUNG). ERN-LUNG is dedicated to providing and supporting the care of patients suffering from rare respiratory diseases on a global scale. It is committed to the prevention, diagnosis and treatment of rare respiratory diseases through very high levels of patient care, education and research.
We are also part of the Clinical Trial Network (CTN), which will give PCD patients access to experimental drugs, the development of which gives much hope. In the case of PCD, drugs have not yet been developed to address the underlying cause of the disease. However, clinical trials do not forget the treatment of complications associated with the underlying disease, which include clinical trials of antibiotics and anti-inflammatory drugs to treat lung infections and inflammation.
Center for highly specialized care for rare liver diseases
Our center is part of the European Reference Network for Rare Liver Diseases (ERN RARE-LIVER). These are highly specialized centers, which were created in order to improve the quality of care for patients with rare diseases and the possibility of mutual international scientific cooperation.
The Motol Center is part of a consortium with the Department of Hepatogastroenterology of the Prague Institute of Clinical and Experimental Medicine (IKEM, www.ikem.cz), which is the largest center for liver disease in the Czech Republic and specializes in the care of patients included in the liver transplant program. The Department of Pediatric Gastroenterology and Hepatology at FNM provides a full range of diagnostic and therapeutic methods and procedures in the field of diseases of the digestive tract and liver. It is an accredited workplace in the field and the largest children's hepatology center in the Czech Republic. It provides care for patients with acute and chronic liver disease, especially patients with biliary atresia, genetic cholestatic disease, including Allagill's syndrome, as well as patients with autoimmune hepatitis, primary sclerosing cholangitis or Wilson's disease.
Center representatives:
FN Motol:
MUDr. Radana Kotalová, CSc., Chief Coordinator of the Center
MUDr. Katarína Mitrová, Ph.D., Deputy Chief Coordinator
MD Marianna Durilová, Ph.D.
MD Eva Vlčková
IKEM:
doc. MUDr. Jan Šperl, CSc., Chief Coordinator of the Center
prof. MUDr. Mgr. Milan Jirsa, CSc., Deputy Chief Coordinator
https://www.ikem.cz/cs/transplantcentrum/klinika-hepatogastroenterologie/a-33/
Dear friends, colleagues, co-workers and sponsors, pediatric patients and their parents!
The Department of Pediatrics of the 2nd Faculty of Medicine of Charles University and the University Hospital in Motol was established in 2004 by merging the work teams of the former I. children's clinic and a significant part of the former II. children's clinic. It is a continuation of their mission - to provide highly specialized and erudite care to children from all over the Czech Republic, whose doctors or parents have requested it. The team of the Pediatric Clinic creates a natural professional background, the "ultimum refugium", for all Czech and Moravian pediatricians, whether they work in children's clinics of teaching hospitals, district children's wards or work as general practitioners for children and adolescents. We are ready to help you and your patients whenever you deem it necessary.
You also meet the staff of the Pediatric Clinic in undergraduate and postgraduate education in pediatrics and its subspecializations, in organizational activities in the care of sick children at the national level and in clinical research and development of biomedical knowledge for the benefit of pediatric patients.
In almost all areas of pediatrics and adolescent medicine, the Pediatric Clinic has highly qualified specialists who provide top diagnostics and therapy - in pediatric nephrology, dialysis and elimination methods, pediatric pneumology and care for children with cystic fibrosis, pediatric endocrinology and diabetology, in pediatric gastroenterology and in the care of children with autoimmune diseases. In cooperation with partner workplaces of the Motol University Hospital, we also provide cardiological, immunological and hematological care.
The credo of the Pediatric Clinic team is "partnership for the benefit of pediatric patients". We are here for you and your patients. Our strength lies in the team experience, in the quality equipment and in the cooperation of the pediatric think tank of the Motol hospital. We strive for straightforward, fast and effective diagnosis and therapy with maximum care for our common pediatric patients.
Our work would be more difficult without sponsors, who make a significant contribution to the renewal and expansion of the clinic's equipment, our "instruments", but also to a friendly and aesthetic environment for our patients. Many thanks to all our sponsors, the clinic team and our patients.
Thanks also go to all Czech and Moravian pediatricians in primary care and inpatient facilities. We highly value their daily endless efforts. It is thanks to them and their work that the sick children who need it most come to us. We thank them for recommending and sending these patients to us. I am sure that it is through our joint efforts that we achieve the maximum possible for the well-being of sick children.
Prof. MD Jan Lebl, CSc.,
on behalf of the team of doctors and nurses of the Pediatric Clinic
The beginnings of the First Children's Clinic in Prague they go back to the history of the old Prague find in Karlov. In 1882, after the division of the University of Prague into a Czech and a German part, a Czech children's clinic was established in the find, whose headmaster in 1885 became associate professor Karel Schwing. This clinic in the building of the foundry in Karlov was marked as clinic for newborns, infants and lactating women.
Successor Swing František was in the role of head clipper, who collaborated with Professor Eduard Babák and published priority papers on energy consumption and respiratory quotient in infants. After Scherer's death in 1916, he ran a clinic for 3 yearsQuit Mann, which has great merits in introducing preventive counseling care for mothers and infants.
He became another leader Karel Švehla, habilitated in 1889, professor since 1924. The clinic dealt mainly with the issue of early childhood, there were a number of contacts with the French and German pediatric schools. In the newly built children's hospital, the establishment of which had the extraordinary merits of prof. Bohdan Neureutter(appointed professor of pediatrics in 1884) took over the Neureutter Clinic Matej Pešina.
The Czech clinic in the find did not have a ward for older children, on the contrary, the clinic in the new children's hospital took care only of older children.
In 1931, prof. Brdlík, pediatrician, who until then ran a children's clinic in Bratislava (there he received great honor by being elected rector of Comenius University, his portrait with the rector's chain hangs in the library of the Pediatric Clinic). His closest collaborator came with him to the find from Bratislava Josef Švejcar, habilitated in 1929 as an associate professor of pediatrics. Because the clinic in the foundry started its activities earlier than the clinic in the children's hospital, proposed by prof. Brdlík mark this clinic as the XNUMXst Children's Clinic. After the departure of prof. Retirement has become Brdlík in 1934 as the head of the clinic located in the Children's Hospital (XNUMXnd Children's Clinic). Švejcar continued to represent him at the 1937st Children's Clinic in Nalezinec, he obtained his professorship in 2. Both Brdlík and Švejcar had a significant influence on shaping the profile of the XNUMXst Children's Clinic before World War II.
During World War II, the university was closed and the Czech children's clinics functioned as a children's department, but the German clinic remained the university clinic. Prof. Hermann Mai, who was preceded by the reputation of the great Nazi, but in the end, as the head of the German clinic, proved positive when he understood what the protectorate was all about, he was transferred to the front!
From 1945, prof. Swiss, II. headed the children's clinic prof. Brdlik. Both clinics were located in the children's hospital building after the war. Only here in the new environment could the clinic of about 100 beds be fully developed, including care for older children. Švejcarová's greatest achievement was her ability to quickly recognize the importance of individual specializations in pediatrics and to find capable and enthusiastic collaborators. Švejcar was also one of the main initiators of the establishment of the Faculty of Pediatrics and the Institute for Child Development Research. The focus remained on infant issues, artificial nutrition research, and cooperation with milk powder producers. A department for the care of premature babies was established at the clinic, and there was good cooperation with maternity clinics in Karlov and later in Londýnská Street. It was a big step forward introduction of school teaching at the clinic, which later resulted in the legalization of a proper hospital school.
It is necessary to pick up from other fields care for allergy sufferers, especially about patients with bronchial asthma. Prof. Polacek developed original approaches to the treatment of childhood toxicos at the time and was also the founder of further subspecialization - pediatric nephrology. After the departure of prof. Švejcar at the newly established ILF clinic at Thomayer Hospital in Krč became prof. Emil Polacek. In 1971, the clinic moved to the Motol hospital. Poláček ran the clinic until his retirement in 1973, when prof. Kamil Kubat. Thanks to him, the long-term careful management of the Čsl magazine was the main reason. Pediatrics, of which he was editor-in-chief. After his retirement, the later professor took over the clinic Zdenka Tresohlava, habilitated in 1978. She dealt mainly with the issue of childhood brain dysfunctions.
From 1989 he was the head of the I. children's clinic until its merging with the II. children's clinic (2004) associate professor and later professor Jan Janda.
The clinic had a total of 110 beds in 5 clinical departments, 2 own laboratories and a complement. The main program was many years of care for low birth weight and pathological newborns in the SP / A department, this department was headed by a later professor Vaclav Mydlil, DrSc and later doc. Peter Zoban, CSc.
The clinic concentrated the most severe patients with bronchial asthma, the founder of the field of pediatric allergology at the First Pediatric Clinic, and in fact there was a later professor throughout the country. Tusk, the allergology laboratory at the clinic was founded by the later doc. He coughed. The Immunology Department of the Motol University Hospital (headed by Stanislava Honzová, MD) and later an independent Department of Clinical Immunology. Pediatric endocrinology was cultivated at a clinic with colleagues by a later professor Lidka Lisa.
Infant medicine has always been one of the "main topic" of the 4st Children's Clinic, Department XNUMXA was headed for many years by an assistant Vojtěcha Špičáková and her successor became a later associate professor Květa Bláhová.
Nephrological issues at the Karlovy Vary workplace were solved mainly by the later prof.Emil Polacek, assistants Miroslav Ort a Maryna Dibelková. After moving to Motol, prof. Poláček by the management of the nephrology department Jan Jandawhen he took over as head of the clinic he became the head of the department as. MUDr.Vladimir Rambousek.
Department 3A, as a mixed department for infants, toddlers and older children, dealt with nutrition and gastrointestinal diseases, and extensive endoscopic activity developed in Motol. A later professor became the head of the department Jiří Neveral.
At the polyclinic of the Motol hospital, the doctors of the 1991st Children's Clinic also ran specialist outpatient clinics - allergological, nephrological, premature and pathological newborns, infants, endocrinological and gastroenterological outpatient clinics. Since XNUMX, he has been included in the XNUMXst Children's Clinic clinical anthropologist (later associate professor) RNDr.Hana Krasničanová.
In individual subspecializations, the clinic has cultivated a number of foreign contacts and research projects (eg Heidelberg, Wien, Hannover, Lyon, Hamburg, etc.).
The clinic's staff initiated the establishment of hobby clubs for children with child dialysis and transplantation, girls with Turner syndrome.
The XNUMXst Children's Clinic was a pioneer in the use of personal computers connected in a network in normal operation, and doc. Pavel Kasal and MUDr. Milan Šikut.
Assistant of the XNUMXst Children's Clinic MUDr. Petr Tláskal CSc. became the head of the children's polyclinic of the Motol University Hospital.
The First Children's Clinic, of course, has always been involved in teaching faculty students, but doctors in individual departments also trained here as part of post-graduate practice. The clinic has been organizing since 1988 foreign exchange practice of medics with offices in Hanover and Freiburg.
After the merger of the 1st and 2nd Children's Clinics, he was the head of the newly established Department of the Pediatric Clinic until 2006 Prof. MUDr. Jan Vavrinec, DrSc. The current advantage is prof. MD Jan Lebl, Csc. After merging the two clinics, the hematology section became a separate department, which joined the Department of Pediatric Hematology and Oncology.
At present, the clinic has 95 beds, of which 12 are intensive care beds. They are divided into 5 wards and an outpatient dialysis-transplant unit for patients with chronic kidney disease.
The tradition of pediatric nephrology at the current Motol Pediatric Clinic begins in the late 40s and early 50s as part of the XNUMXst Children's Clinic of the Children's University Hospital in the area of Charles University in Prague. A close collaborator of prof. Josef Švejcar became doc. Emil Poláček, who was intensely interested in the issue of water and electrolyte metabolism in children. It was based on the work of American and British physiologists and pediatricians. As part of the development of the child at the time, experiments with the treatment of dehydration were also carried out, in which the signatory actively participated as a demonstrator or auxiliary scientific force during their studies. At the time of the recurrence of severe diarrheal epidemics caused by enteropathogenic E. coli, which were associated not only with significant morbidity but also mortality (including acute renal failure), Poláček was a pioneer of parenteral treatment with infusion solutions. It spread relatively quickly to children's wards in the former Czechoslovakia and significantly improved the prognosis of sick children.
Since the 60s, MUDr. Miroslav Ort, later an assistant at the First Children's Clinic, of the secondary physicians, MUDr. Maryna Dibelkova, MD Jaroslava Tolarová and aspirant MUDr. Ivana Reneltová, later working at IKEM in Krč. Renal biopsies of children began to be performed at the clinic, which was evaluated by the then assistant of the Institute of Pathological Anatomy, MUDr. Josef Stejskal. Very soon, the team embarked on active treatment of acute renal failure by peritoneal dialysis, in this regard, several reports were published abroad, which were among the first in this area.
Prof. Poláček took over the management of the clinic after the departure of prof. Švejcar to the ILF clinic in Krč and also led the 1973st children's clinic after moving to Motol until the new head, prof. Kamila Kubáta in 1973. In 1972, Poláček's monograph Children's Nephrology was published, which was the first detailed textbook of this subspecialization. In XNUMX he joined the XNUMXst Children's Clinic, already in Motol, MUDr. Jan Janda, who was prof. Poláček was appointed as an assistant professor to lead the teaching and continue the already established activities. Contact with German nephrologists (Uni-Kinderklinik Charité, Berlin, then GDR) and Janda with MUDr. Jiří Kreisinger and MUDr. Květa Bláhová systematically started preparing a treatment program for chronic kidney failure by dialysis and transplantation. Of the clinic's staff, the two above-mentioned secondary clinics and a team of nurses were mainly involved in the implementation of this treatment.
The first kidney transplant in a child in the Czech Republic was performed at IKEM in 1977 after previous preparation by peritoneal dialysis. Medical and nursing staff trained at the workplace on an artificial kidney, first at the center for adults with prof. The war in Strahov. We started dialysis in 1980 and the first transplant in Motol was performed in 1981 in cooperation with MUDr. Jaroslav Špatenka from the Motol Children's Cardiac Center and Doc. Kočandrle from IKEM. Then the kidney replacement program continued successfully, the authorized employee of the children's dialysis center was for many years MUDr. Jiří Kreisinger, later assisted by MUDr. Milan Šikut, from the beginning of the activity until today, the sister team is led by the station nurse Eva Pavlínová-Vlachová.
Later, MUDr. Eva Šimková, who has been working temporarily at the children's clinic in Belfast since 2006, has been led by the dialysis team since 2006 by MUDr. Karel Vondrák. Thanks to the extensive financial support of sponsors (eg the Medical Helpline Foundation and Princess Therese von Schwarzenberg and the Archa Chantal Foundation, Mrs. Chantal Poulain), the S1B section was reconstructed in 2000 and especially improved the "design" of the dialysis unit and ambulance.
There has always been close cooperation between the nephrology department and the team of Motol pediatric urology, with which nephrology-urology issues are addressed together. Pediatric urology was cultivated at the Children's Surgical Clinic of the Karlov complex (Prof. Kafka, later Dr. Helena Faflová, Doc. Milan Krolupper, CSc.). The latter was a popular conciliator for many years after the relocation of pediatric surgeons to Motol and also participated in the introduction of kidney transplantation.
The clinic has always had an extensive nephrology outpatient clinic, in which virtually all physicians in the nephrology department participated. And II. children's clinic in Motol cultivated pediatric nephrology later Prof. MUDr. Jiří Švorc, his close collaborator was as. MUDr. Jiří Dušek, CSc., Both later went to the propaedeutic clinic of the Pod Petřínem Hospital. Several members of the pediatric nephrology team spent more time in the nephrology section of the Uni-Kinderklinik in Heidelberg (Prof. Karl Schärer, Prof. Otto Mehls). MUDr. Milan Šikut, MD Janusz Feber, MD Tomáš Seeman, the last two of those named later habilitated at the faculty. Doc. Feber has been working at the Children's Clinic in Ottawa, Ontario, Canada in recent years. Doc. Seeman is currently the head of the children's transplant program in Motol and works closely with the Motol University Hospital Transplant Center.
The Nephrology team of the Pediatric Clinic is currently solving complex issues of kidney and urinary tract diseases in cooperation with other departments of the Motol pediatric department (urological group of the Department of Pediatric Surgery, Motol University Hospital (head Jaroslav Špatenka, MD, CSc. , ARK, etc. As part of the purification methods, the elimination method by plasmapheresis was introduced at the clinic and in the last 2 years in indicated cases as the only pediatric workplace in the Czech Republic also immunoadsorption.
The inpatient nephrology and dialysis department of the clinic is located in section 1C, where children with nephropathy and uropathies are hospitalized, there is close cooperation with the pediatric urology section of the Department of Pediatric Surgery at Motol University Hospital (Jiří Morávek, MD, Zeman, MD, Jan Kříž, MD) . The nephrology clinic is located in section 3E. Today, chronic renal failure in children is treated in most cases by peritoneal dialysis using automatic devices (so-called cyclers). Due to the use of artificial kidney devices, we had to accept that adult patients are also dialyzed in the children's dialysis unit.
In the premises of 3E, there is an extensive nephrology outpatient clinic, which, of course, mainly concentrates patients with renal dysfunction, who are candidates for a dialysis-transplant program. Otherwise, this ambulance represents a counseling facility for the catchment area, but complicated cases from all over the Czech Republic are also concentrated here within the counseling activities. Of course, mainly children from the Czech Republic are preparing for transplantation, but we also perform it on smaller children and complicated children from Slovakia. Since 2001, in addition to kidney transplants from cadaveric donors, transplants from living donors, mostly parents, have been performed.
The staff of the nephrology department participated in the establishment of the annual Working Days of Pediatric Nephrology, the first event was held in Třeboň in 1980. Children's nephrologists from Motol also hold leading positions in the working group committee for many years.
Important sponsors of the Pediatric Clinic
The staff of the Pediatric Clinic expresses their sincere thanks to all the sponsors of the clinic. As in every developed country, the sponsors in the Czech Republic represent a significant contribution to the replacement and expansion of the equipment of individual workplaces and to ensuring a friendly environment for children's patients.
Sponsors:
- Fond Sidus, ops
- E.ON IS Czech Republic sro
- Mrs. Jančová
- Ing. Log
- Novo Nordisk, sro
- Mrs. Vodrážková
- NF Drop of Hope
- Euroforce - CZ, spol. sro
- Swedish Orphan Biovitrum sro
- CRESTYL management as
- Mrs. Řebřinová
- Cystic fibrosis patients club, os
- Mrs. Dědková
- KB Nadace Jistota, as
- Dun & Bradstreet, Ltd. sro
- FIOMO, as
- CRESTYL REAL ESTATE, SRO
- HUTS Opava, as
- HUTS development, sro
- Best Medialni spolecnost, sro
- A.IMPORT. CZ spol. sro
- Profimedia. CZ sro
- Sylab Czech sro
- Motolák, student association of the 2nd Faculty of Medicine, Charles University in Prague
- Mr. Freedom
- Ing. Cubic
- Mrs. Vanišová
- Mrs. Frank
- Mr. Smaha
- ROCHE sro
- Wine Food Market Ltd.
- Mr. Kročen
- OK systém sro
- Mrs. Dědková
- TOP secutity sro
- Bronda Games Ltd.
- Computer Systém Praha spol. sro
- DEMAX sro
- Fresenius Medical Care - CR, sro
- AWD - Stiftung Kinderhilfe
- A care as
- Beiersdorf spol. sro
- Ing. Street
- Bc. Dvořák
- CYBER GLOBAL sro
- Life for children ops
- Mr Habásko
- AC Sparta Prague football, as
- Mrs. Kowalski
- Chiesi CZ sro
- NOKIKA sro
- PAIRAM Solution sro
- M.Sc. The church
- Conseq Investment Management, as
- PhDr. Shoemaker
- Privileges Services sro
- Spolek Every basket helps, os
- Alza. cz as
- Roger Napier DUNLOP
- Ing. Hajková
- NF Green Life
- Mr and Mrs Anders and Lena Kornblad
- Mr. Sellers
- KLARO, SPOL. sro
- Technologie Kozlík sro
- HARIBO CZ sro
- Marks & Spenser Czech Republic as
- Lindt & Sprüngli sro
- Horse and Glamor sro
- Ing. Krivánková Beranová
- Nestlé Česko sro
- Socialbakers as
- Dr. Max Pharma sro
- NF Pink Bubble
- BAXTER CZECH spol.sro
- Unit and Sofa sro
- T-Soft Eternity Foundation
- Mrs. Shaw
Information for sponsors
The sponsors represent a significant contribution to the replacement and expansion of the equipment of individual workplaces as well as to ensuring a friendly environment for pediatric patients. If you are considering whether to provide us with your support, then know that the money will be handled responsibly. Your help will directly translate into better treatment, diagnosis and care options for pediatric patients.
With the possible support of our clinic, you will find yourself in good company.
Sponsor us:
Motol University Hospital
based: V Úvalu 84, 150 06 Prague 5 - Motol
Represented by: JUDr. Ing. Miloslav Ludvík, MBA, director
ID: 00064203
Tax ID CZ00064203
Bank connection: Czech National Bank
account number: TBU
variable symbol: 2126
(variable symbol distinguishes the Pediatric Clinic from other workplaces within the hospital)
Doctors
Knowledge:
head - Prof. MUDr. Zdenek Sumnik, Ph.D.
Chief Medical Officer – primary doc. MD Štěpánka Průhová, Ph.D.
head nurse - Mgr. Jana Boháčová
Working groups, inpatient departments, outpatient clinics and laboratories of the Pediatric Clinic:
- pediatric nephrology working group with inpatient department and outpatient clinic - head doc. MUDr. Jakub Zieg, Ph.D.
- inpatient department of pediatric nephrology - head doc. MUDr. Jakub Zieg, Ph.D., station nurse Mgr. Petra Janásová
- Department of Dialysis and Elimination Methods - Head MUDr. Naděžda Šimánková, station nurse Eva Vlachová
- pediatric nephrology clinic - head MUDr. Naděžda Šimánková
- working group of pediatric pneumology, allergology, cystic fibrosis and cardiology and the inpatient ward, outpatient clinics, endoscopic examination rooms and laboratories - head prof. MUDr. Petr Pohunek, CSc.
- inpatient department of children's respiratory diseases - head MUDr. Tereza Doušová, station nurse Hana Benešová
- cystic fibrosis center - head of the clinical part MUDr. Veronika Skalická
- lung functional diagnostics laboratory - head prof. MUDr. Petr Pohunek, CSc.
- cardiology outpatient clinic and ECG laboratory - MUDr. Veronika Stará
- working group of pediatric endocrinology, diabetology and autoimmune diseases with inpatient department, outpatient clinics and laboratories - head prof. MUDr. Jan Lebl, CSc. and prof. MUDr. Zdenek Sumnik, PhD.
- inpatient department of pediatric endocrinology and diabetology - head prof. MUDr. Zdeněk Šumník, PhD., Station nurse Radomíra Kučerová
- outpatient department of pediatric endocrinology, diabetology and anthropology - head MUDr. Stanislava Kolouskova, CSc.
- molecular genetics laboratory - head prof. MUDr. Ondrej Cinek, PhD.
- working group of pediatric gastroenterology, hepatology and nutrition with inpatient department, endoscopic examination rooms, ambulances and laboratories - head doc. Jiří Bronský, MD, Ph.D., station nurse Jitka Doubravová
- inpatient department of infant medicine with an ambulance - head doc. MUDr. Květa Bláhová, CSc., Station nurse Jiřina Mašková
- intensive care unit of the Pediatric Clinic inpatient department - chief physician doc. MUDr. Filip Fencl, Ph.D., station nurse Ivana Hindráková
Working groups
- pediatric nephrology working group with inpatient department and ambulances
- inpatient department of pediatric nephrology
- workplace of dialysis and elimination methods
- pediatric nephrology clinic
- working group of pediatric pneumology, allergology, cystic fibrosis and cardiology and the inpatient ward, outpatient clinics, endoscopic examination rooms and laboratories
- inpatient department of childhood respiratory diseases
- pediatric pneumology clinic
- allergy clinic
- cystic fibrosis center
- lung functional diagnostics laboratory
- ciliary epithelial function laboratory
- ECG laboratory and cardiology outpatient clinic
- working group of pediatric endocrinology, diabetology and autoimmune diseases with inpatient department, outpatient clinics and laboratories
- inpatient department of pediatric endocrinology and diabetology
- inpatient workplace of autoimmune diseases with an outpatient clinic
- outpatient department of pediatric endocrinology, diabetology and anthropology
- molecular genetics laboratory
- laboratory of autoimmune diseases
- working group of pediatric gastroenterology, hepatology and nutrition with inpatient department, endoscopic examination rooms, ambulances and laboratories
- a comprehensive care center for children with developmental disorders and their families
Nephrology and dialysis
The inpatient part of the nephrology department of the Pediatric Clinic of the University Hospital is located in the children's monoblock at ward 1C (headed by doc. Jakub Zieg, MD, Ph.D.). In addition, patients under 1 years of age are hospitalized in the PC department (headed by Květa Bláhová, MD, CSc., Who systematically deals with nephro-urological issues in children of this age group). The nephrology team provides comprehensive diagnosis and treatment of children with kidney and urinary tract diseases. He works closely with other subspecializations at the Motol Hospital (Department of Pediatric Surgery, Department of Imaging Methods, Transplant Center, Department of Endocrinology and Nuclear Medicine, etc.).
The clinic addresses the issue of acute renal failure, chronic renal failure and chronic renal failure, including transplantation. The department provides services to children and adolescents from the catchment area, but in many cases it takes care of children from all over the Czech Republic. This is often the case in children with acute renal failure, in children with chronic renal impairment. Kidney transplants in patients under the age of 19 are performed throughout the Czech Republic only in Motol, and small children from Slovakia are also transplanted there. Doc. MUDr. Jakub Zieg, Ph.D. is currently the head of the children's transplant program in Motol and works closely with the Transplant Center of the Motol University Hospital.
The dialysis center at section S1B (currently headed by Karel Vondrák, MD) is equipped with modern instrumentation (artificial kidneys, devices for plasmapheresis, immunoabsorption, devices for home peritoneal dialysis, bone densitometer, ultrasound device, equipment for urodynamics examination). The activities of the counseling nephrology outpatient clinic are extensive. In addition to classical nephrology, the team deals with the issue of hypertension in children and in this sense acts as a pediatric reference center for the Czech Republic.
The department also concentrates large groups of patients with polycystic kidney disease, familial nephropathy, nephrotic syndrome, etc. There is an endowment fund for children with renal impairment, and an instructive information brochure has been issued for parents of sick children. The team's doctors are the main authors of the publication Pediatric Nephrology, which was published in 2006, and also worked on children's nephrology issues for the Repetitorium. Our department also provides annual Children's Nephrology Working Days, for which abstracts in Czech and English are published.
Colleagues from all over the Czech Republic are preparing for the department, who are preparing for certification in pediatric nephrology. From Motol, she is led by the staff of our team as well Children's Nephrology Working Group website.
Within the subspecialization, a number of grant projects and research plans are being addressed on an ongoing basis, and the department is involved in international studies that test the effectiveness of immunosuppressive therapy and the effect of hypertension on the progression of renal dysfunction. For more than 15 years, there has been cooperation with top institutions in pediatric nephrology in the Federal Republic of Germany (participation in studies, joint publications).
Pediatric pneumology
The Working Group for Pediatric Respiratory Diseases of the Pediatric Clinic participates in inpatient and outpatient care for children with respiratory and allergic diseases. The working group has the beds of ward 1A and uses other beds within the clinic for the hospitalization of some patients. Children with acute respiratory diseases are admitted to inpatient care, as well as patients for comprehensive diagnostic care or patients with chronic diseases of the respiratory tract who require inpatient care.
A large number of patients are treated in outpatient clinics, where patients come for pneumological diagnosis and medical care. As part of comprehensive care for respiratory diseases, there is a modern and comprehensively equipped laboratory for functional examination of the lungs in children and adolescents, where several dozen patients are examined daily. A methodology for examining lung function in uncooperative children, newborns and infants is also being introduced.
The care also includes an above-standard equipped children's flexible bronchoscopy center, where we perform approximately 200 procedures per year. The number of performances makes this center one of the most active in Europe. For this reason, our center is involved in the program of European education and international courses in pediatric bronchology within the European Respiratory Society (ERS). We also provide bronchoscopic service for other departments and clinics of the Motol University Hospital; we also perform flexible bronchoscopy in intensive care units and neonatology workplaces in other Prague workplaces. The department is the only one in the country to provide a complete examination of ciliary motility disorders according to the latest ERS recommendations, including equipment for high-speed video microscopy and electron microscopy. We also provide pH metric diagnostics. We provide superconsulting care in the field of respiratory diseases for workplaces from all over the country.
The main problems the working group deals with are obstructive diseases (bronchial asthma and its differential diagnosis), acute and chronic inflammatory diseases of the bronchi and lungs, interstitial lung diseases. We provide follow-up care for patients with congenital defects of the respiratory tract and patients after severe acute illnesses.
The workplace includes a center for the care of cystic fibrosis patients, which cares for 370 patients and shares many other patients with workplaces outside Prague. The center includes a laboratory for examining the concentration of chlorides in sweat, which performs around 2000 sweat tests per year. In cooperation with the Institute of Biology and Medical Genetics, it also provides comprehensive molecular genetic diagnostics of cystic fibrosis. The center works according to European standards of care for patients with cystic fibrosis and provides and manages long-term multidisciplinary care for these patients. It participates in the European Union's ECORN-CF (European Centers of Reference Network for Cystic Fibrosis) and EuroCareCF (European Coordination Action for Research in Cystic Fibrosis) programs and cooperates with a number of foreign workplaces. The Center also cooperates with RAPSODY (Rare Disease Patient Solidarity) and its umbrella organization EURORDIS (European Organization for Rare Diseases). There is also close cooperation with the Cystic Fibrosis Patients' Club.
The working group is also active in terms of publications and science, currently solving two subtasks of the research plan of the Ministry of Health of the Czech Republic and several grant tasks. Members of the working group participate in teaching in undergraduate and postgraduate studies. The department holds an accreditation for postgraduate education in the field of pediatric pneumology.
Endocrinology
Children's Diabetes Center of the Pediatric Clinic of the Motol University Hospital
The inpatient diabetology department, together with the outpatient clinic, is the largest and largely unique facility of its kind in the Czech Republic. The focus of our work is undoubtedly comprehensive care for children with type 1 diabetes, which is the most common type of childhood diabetes. However, in cooperation with the Molecular Genetics Laboratory, we are also successfully developing a program for the diagnosis and treatment of children with other types of diabetes occurring in childhood, especially MODY, neonatal diabetes, etc. Members of our clinical team are physicians with many years of experience with modern diabetes current trends in pediatric diabetology, as well as educational nurses, whose role in the successful treatment of diabetes in children is completely irreplaceable and in many respects even more important than medical care, as well as psychologists, cooperation with whom we have repeatedly proved successful, especially in difficult-to-compensate children. We are convinced that only teamwork can celebrate success in the treatment of such a complex chronic disease as childhood diabetes.
The basic precondition for the optimal treatment of diabetic children is, in addition to their own clinical practice, also regular monitoring of novelties that appear in the field of childhood diabetes and their rapid introduction into clinical practice. We are pleased to be able to offer these new opportunities to our patients at virtually the same time as is common in developed European countries. We are succeeding thanks to long-term and close cooperation with the world's centers for childhood diabetes, whether in multicentre scientific studies or on the basis of numerous personal ties. It is also a very gratifying fact that the work from our molecular genetics laboratory under the leadership of prof. MUDr. Ondřej Cink, Ph.D. colleagues from foreign workplaces are highly valued. The same words can also be said about the Czech Register of Childhood Diabetes, which has been working at our clinic for more than 15 years and is one of the best in Europe due to its completeness. Thanks to grants from the Kingdom of Norway, research is currently underway at our clinic monogenic diabetes in children.
Projects Childhood diabetes was established in cooperation with the Czech Diabetological Society JEP and with the support of the Ministry of Health of the Czech Republic from the chapter National Action Plans and Concepts. The aim of the project is to increase the awareness of diabetic children and their parents, as well as the general public about childhood diabetes. It strives to provide up-to-date information targeted at this age group.
Endocrinology department and outpatient clinic
The pediatric clinic's working group of pediatric clinics covers with its experts the whole spectrum of endocrine diseases that we encounter in children. Our main focus is on growth disorders (growth hormone treatment center is the largest in the Czech Republic in terms of the number of treated children by far), puberty disorders (including comprehensive treatment of premature puberty with modern drugs), adrenal diseases, cerebral palsy, parathyroid glands, thyroid and metabolic bone diseases. We work closely not only with general practitioners for children and adolescents, but also with other workplaces at the University Hospital in Motol and together we provide care and support for children with primary endocrine diseases, but also with multiple difficulties and problems, including endocrine disorders. In addition to experienced clinical endocrinologists, our team also includes experts from the anthropological outpatient clinic, with whom we consult especially the most difficult patients with growth and development disorders. Needless to say, both parties benefit from this cooperation.
Gastroenterology and nutrition
The Gastroenterology Department of the Pediatric Clinic deals with complex diagnostics and treatment of diseases of the digestive system and liver. It is an accredited workplace in this field. Diagnostic upper and lower endoscopy of the gastrointestinal tract, sclerosing of esophageal varices, removal of foreign bodies and polyps and esophageal pH-metry are performed here. Thanks to the instrumentation, these examinations can be performed on even the smallest infants.
The department is particularly focused on the diagnosis and treatment of idiopathic inflammatory bowel diseases, and there is an extensive registry of these patients at the clinic. The department has also been dealing with malabsorption syndrome for several decades, especially issues of celiac disease, its enterobiopsy and serological diagnosis. The ward diagnoses and treats children with severe liver disease, and concentrates patients before and after liver transplantation.
The department was granted the status of a workplace with professionally guaranteed care for patients with chronic viral hepatitis by the Czech Society of Hepatology. The department has also been involved in the health and health of children for many years. Long-term enteral and parenteral nutrition, including home parenteral nutrition, is performed medically. In indicated cases, endoscopic percutaneous gastrostomy is performed, with which there is many years of experience.
List of physicians and contacts
Head:
Prof. MUDr. Zdenek Sumnik, Ph.D.
tel .: 224 432 000, 224 432 001
fax: +224 432 020 XNUMX
Email: zdenek.sumnik@fnmotol.cz
Chief Physician:
doc. MD Štěpánka Průhová, Ph.D.
phone: 224 432 003
Email: stepanka.pruhova@fnmotol.cz
List of doctors
name: | Email: | teaching: |
MD Shenali Amaratunga | ||
MD Jana Bartošová | University | |
doc. MUDr. Kveta Blahova, CSc. | University | |
prof. MD Jiří Bronský, Ph.D. | University | |
prof. MUDr. Ondrej Cinek, Ph.D. | University | |
MUDr. Ivana Copova | ||
MD Tereza Doušová | University | |
| MUDr. Mariana Durilova, Ph.D. | gastroped@fnmotol.cz | |
doc. MD Filip Fencl, Ph.D. | University | |
MD Eva Flachsová | ||
MD Eva Fürstová | ||
MD Katerina Gregorová | ||
doc. MUDr. Ondrej Hradsky, Ph.D. | University | |
MD Denis Kazek | ||
M.Sc. Aneta Kodytková | yep | |
MUDr. Stanislava Kolouskova, CSc. | University | |
MD Patrik Konopásek | ||
RNDr. Hana Kosek, CSc. | University | |
MUDr. Radana Kotalova, CSc. | University | |
MUDr. Vaclav Koucky, Ph.D. | University | |
MD Vlasta Krejčová | ||
| MUDr. Jana Krenek Malikova, Ph.D. | jana.malikova@fnmotol.cz | University |
MD Michal Kubát | ||
| MD Šárka Kusáková | sarka.kusakova@fnmotol.cz | |
MD Tereza Lerchová | ||
MD Petra Lesná | ||
MD Alexandra Liptáková | ||
M.Sc. Klara Maratová | yep | |
MD Vendula Martinů | University | |
MD David Meguinet Chucesov | ||
MUDr. Katarina Mitrova, Ph.D. | ||
MD Vit Neuman | ||
prof. MD Jiří Neveral, CSc. | University | |
MD Barbora Obermannová, Ph.D. | ||
MD Lenka Petruzelová, Ph.D. | University | |
MD Lukáš Plachý | ||
prof. Petr Pohunek, CSc. | University | |
Doc. MUDr. Stepanka Pruhova, Ph.D. | University | |
MD Veronika Skalická | University | |
doc. MUDr. Ondrej Soucek, Ph.D. | University | |
MD Old Veronica | ||
MD Vojtěch Šedivý | ||
MD Nadezhda Šimánková | University | |
doc. MD Marta Šnajderová | University | |
prof. MUDr. Zdenek Sumnik, Ph.D. | University | |
MD Eva Švábová | ||
MD Ledjona Toni | ||
MD Žofia Varényiová | ||
MD Karel Vondrák | University | |
RNDr. Daniela Zemkova | ||
doc. MD Jakub Zieg, Ph.D. | University | |
MD Jan Zikan |
Information for patients
The Pediatric Clinic of the Motol University Hospital is a specialized pediatric institution which, in addition to medical and preventive care for young patients, also deals with teaching and research. Due to the high professional level of its physicians, the clinic ranks among the so-called "supraconsiliary workplaces" - it normally acts as an advisory body for other workplaces and physicians who may need advice or professional guidance in some very complex and rare care situations for pediatric patients.
The clinic has 90 beds, of which 30 are intensive care beds. They are divided into 5 departments and an outpatient dialysis-transplant unit for patients with chronic kidney disease. The clinic also includes a gastroenterology laboratory and a laboratory for molecular genetics.
You can find contacts for individual workplaces in the section Contact , more about individual working groups can be found in the tab Working groups.
Hypertension
Prepared by: Prof. MUDr. Tomas Seeman, CSc.
You can also download the text <a href="https://cdn.shopify.com/s/files/1/1932/8043/files/200721_ODSTOUPENI_BEZ_UDANI_DUVODU__EN.pdf?v=1595428404" data-gt-href-en="https://en.notsofunnyany.com/">here</a>.
1. What is hypertension?
Hypertension is increased blood pressure. In childhood, hypertension means blood pressure that exceeds the normal blood pressure of healthy children of the same sex, age and height with at least 3 repeated measurements on 3 different days. The 95th percentile of a healthy child population is considered to be the limit of normal blood pressure, ie. that 95% of children of the same sex, age and height have lower blood pressure than this limit. The specific blood pressure limit for a particular child can be found in the percentile blood pressure charts that are part of the child's Health and Vaccination Card.
2. What causes hypertension in children?
Hypertension in children is most often caused by some other disease (so-called secondary hypertension), especially kidney disease (so-called renal hypertension), renal arteries (so-called renovascular hypertension), endocrine glands (so-called endocrine hypertension) or heart and blood vessel anomalies . Thus, in this case, hypertension is not a separate disease, but only a manifestation of some other disease.
On the contrary, in adolescents, as well as in adults, the most common cause is the so-called primary (or essential) hypertension, when children have all healthy organs, they have "only" increased blood pressure. The exact cause of primary hypertension is not known, the factors of internal - hereditary disposition and influences of the external environment, especially eating and exercise habits, play a role in its occurrence.
3. How common is hypertension in children?
In childhood, hypertension occurs in 1-3% of children, which is 10-30 times less common compared to the incidence of hypertension in adults, but it still follows that every thirtieth to one hundred children suffer from hypertension.
4. What makes hypertension dangerous?
Hypertension is one of the most important risk factors for cardiovascular disease, such as myocardial infarction, stroke or heart failure, which are the most common cause of death in adult patients. This means that patients with high blood pressure have more frequent heart attacks and strokes than patients with normal blood pressure, and also die more often and earlier. Hypertension is therefore nicknamed the "silent killer" because patients do not hurt, but kill them. This is treacherous for her and thus increases her danger.
Also in childhood, hypertension is associated with an increased incidence of cardiovascular damage in the general pediatric population as well as increased mortality from cardiovascular disease in chronically ill children, such as chronic kidney failure. Hypertension is also one of the most important risk factors for worsening chronic kidney disease, ie children with renal impairment and high blood pressure reach chronic renal failure with the need for dialysis (artificial kidney) and transplantation before children with normal blood pressure.
5. How does hypertension manifest itself in children?
Hypertension is most often not a problem in children. That's treacherous about her. If difficulties occur, hypertension usually lasts for a long time or is very severe. Typical problems with hypertension include headaches, nosebleeds, fatigue, increased sweating, loss of appetite and failure in young children.
Because hypertension is most often asymptomatic in children, it is often detected during a preventive examination by a general practitioner for children and adolescents.
6. How is it found that my child has hypertension?
Very simply - by measuring blood pressure. Therefore, it is recommended that children measure their blood pressure whenever a child has any problems that may be caused by hypertension (see section 5). However, as hypertension often does not cause any problems in children, it is recommended that all children have blood pressure measurements, even if they do not have any problems, at each preventive check-up with a general practitioner for children and adolescents from the age of 3 years. Part of the Health and Vaccination Card of each child (see www.babyonline.cz/pece-o-dite/zdravotni-a-ockovaci-prukaz.html), which every child has received since birth since 1994, are graphs with normal blood pressure values, from which it can be determined whether the child's blood pressure appears to be normal or elevated.
7. What needs to be examined if my child develops hypertension?
When examining a child with hypertension, it must be found out:
1) whether it is real hypertension or just the so-called "white coat hypertension", ie the phenomenon when the child has high blood pressure only in the doctor's office, but at home his blood pressure is normal. Therefore, we will measure blood pressure at home several times or the doctor will perform 24-hour monitoring of the child's blood pressure at home using a special blood pressure monitor.
2) why does the child have hypertension - is it primary or secondary hypertension? Doctors use examinations that include urine, blood and ultrasound (sonographic) examinations of the kidneys and heart,
3) whether the child does not already have an affected heart or kidney with increased blood pressure,
4) whether the child has other risk factors for cardiovascular disease in addition to hypertension, especially increased blood fat levels, overweight or obesity.
8. How is hypertension treated in children?
If it is revealed that hypertension is caused by some other disease, ie. that it is the so-called secondary hypertension, there is always an effort to treat the underlying disease (especially kidneys, endocrine glands), which causes hypertension. If the underlying disease can be cured, hypertension will also disappear.
If hypertension does not cause subjective discomfort to the child or the child is not found to have secondary hypertension (ie, especially kidney disease) or hypertensive heart or kidney disease, hypertension is treated with regimen measures (without medication). These include, in particular, a reduction in overweight / obesity (a high-calorie diet that corresponds to the child's energy expenditure and does not exceed it), a reduction in dietary salt intake (given that most salt is taken in the form of prepared meals). reduction of consumption of ready-made foods with a high salt content - eg "fast food" meals, powdered soups, cold cuts, potato chips, sticks, nuts, burgers) and increased physical activity (dynamic activities - fast walking, running, cycling) , swimming, at least 3 times a week).
If a child's hypertension is causing the child subjective difficulties or the child has already had kidney disease or hypertension, the heart must be treated with hypertension from the beginning with antihypertensive drugs (so-called antihypertensives). Currently, there is a large selection of antihypertensive drugs for children, so it is usually not a problem to reduce high blood pressure.
Treatment of hypertension clearly leads to an improved prognosis of children with hypertension of the future - ie if they are well treated in the future they will not be at risk of serious heart, blood vessel or kidney disease.
Further information for patients and parents of pediatric patients with hypertension is available in Czech, English or German on the websites of various professional societies, such as:
https://www.pediatrichypertension.org
Prague, March 2011 Prof. MUDr. Tomas Seeman, CSc.
Department of Pediatrics, University Hospital in Motol and 2nd Faculty of Medicine, Charles University in Prague
Monogenic diabetes in children
You can download information on the diagnosis and treatment of monogenic diabetes <a href="https://cdn.shopify.com/s/files/1/1932/8043/files/200721_ODSTOUPENI_BEZ_UDANI_DUVODU__EN.pdf?v=1595428404" data-gt-href-en="https://en.notsofunnyany.com/">here</a> (ppt presentation [723kB]).
The growth and maturation of the child
Author Prof. MD Jan Lebl, CSc.
Download full text: The growth and maturation of the child [doc; 185,9 kB]
The emergence of a new life
One celebrates a person's life every year. However, over a cake with candles or a bottle of champagne, opened in honor of the anniversary of his birth, he does not realize that his life arose three quarters of a year earlier. That was when his identity was born, his distinctive and unmistakable personality.
New human life begins when one of a large number of sperm penetrates in close proximity to an egg, penetrates its shell, and introduces its contents into it - 23 paternal chromosomes. They thus attach to similar 23 maternal chromosomes. This is the moment of fertilization, conception.
In a short time of conception, she decides whether the new life will take the form of a woman or a man. If the sperm brought a chromosome called an "X", the future little man will be a girl. If she brought the "Y" chromosome, she'll be a boy. At the same time, the moment when the sperm merges with the egg also decides what inherited traits the future person will bring into the world. Both egg and sperm chromosomes carry a huge number of genes. Genes contain information about all the inherited traits of a new human in chemical form, deoxyribonucleic acid for short. Thanks to its genes, the child will have part of his innate traits from his mother and part from his father. He has it written in his genes if he has blue or brown eyes and blond or dark hair. There is information about how big he will be and what his temperament will be. Genes also provide the basic preconditions that will co-decide in the future whether a child will be successful in school, whether he will have a musical talent, and what spatial imagination he will need in mathematics. We suspect that they also record how long his life is likely to be and whether he will be at risk of some common health problems at a mature age, such as high blood pressure, diabetes or cancer. These vital reports have been recorded in its 46 genetic information carriers since its inception.
Soon after fertilization, the egg begins to divide first into two, then into four, eight and more and more cells. With each subsequent cell division that follows, the same set of 46 chromosomes doubles and passes to all emerging cells. Each cell of the new person's future body will contain the same 46 chromosomes. Throughout our long lives, each of us will carry with us half of the genetic information obtained from our mother and half from our father.
At the moment of conception, therefore, all the inherited qualities of the future person are decided. In this sense, we, the parents, continue to live in our children: It is the combination of our chromosomes, our genes that makes our child unique, that persists in him and will later be passed on to more and more generations. Like us ourselves, we are in our genes the successors of our own parents, grandparents, great-grandparents ... during the horrors of the Thirty Years' War or during the national awakening in the 19th century. In terms of our genes, the history of mankind is also our personal history, the future of the human race and our personal future.
In our children as parents, we continue to live not only in this biological sense. We already know that the inherited qualities of the new man were decided by the moment of conception. We entered the selection of these traits for our child by choosing our parenting partner, the child's second parent. From the moment of conception, we have a long period together with the baby, which will first grow in the mother's womb, after birth already here, visibly, next to us. We will gradually pass on our knowledge, skills, our worldview, our values and ideals. We will bring him up to our image. Feeling and understanding for a small and gradually growing person will tell us what he needs from us at any given time. Our child will be our successor thanks to everything we teach him.
Based on the inherited qualities and abilities of our child, we will build the basis of his future unique personality, his most individuality, through daily contact. In the end, we may not be completely satisfied with our educational work, but it already belongs to the parental fate. If there was a recipe for a perfect upbringing, we would be surrounded by perfect human beings and life would be too monotonous.
Summary: New human life arises at the moment when the paternal sperm merges with the mother's egg. At that moment, 23 pairs of chromosomes from my father connect with the same number of chromosomes from my mother. This set of chromosomes is transferred to all cells of the future human. Chromosomes contain genes that carry genetic information. At the moment of conception, it is decided not only about the sex, but also about all the inherited traits of the new person.
Innate and acquired traits
What qualities, abilities and skills of a person are innate and which can his loved ones influence by upbringing? People have been dealing with this issue since ancient times. At first, it was only possible to speculate about this problem. Over the last century, reflections on the share of innate and acquired human characteristics have gained a more rational basis thanks to new findings in the biological and psychological sciences.
At the beginning of the twentieth century, one of our most important natives formulated his developmental theories, Sigmund Freud (1856-1939), originally from Příbor in Moravia. He is considered the founder of psychoanalysis, but he was also a great expert in developmental psychology, ie the psychology of individual life periods. He greatly emphasized the influence of the child's early emotional experiences, in the first weeks and months of life, on the further development of his personality. He considered the influences from the immediate surroundings, which are mediated by parents and other family members, to be essential for the development of the child's mental world. His teaching of psychoanalysis is based on the assumption that this period is the basis of possible future mental problems of man.
A little later, a Swiss psychologist Jean Piaget (1896-1980) used new knowledge of biological sciences. He hypothesized that the development of nervous system cells and the gradual formation of individual parts of the brain that occur during a child's life predetermine both the development of his mental abilities and his emotional life. He considered the influence of hereditary, innate characteristics of the brain to be paramount. He judged that the maturation of brain cells is a prerequisite for acquiring new skills and for broadening the child's mental horizon. Piaget considered the impact of the environment to be insignificant.
In recent decades, the knowledge of both biological and psychological sciences has continued to grow. Thanks to them, we again understand the role of the environment in the development of a small person. A negative example may be the impaired development of children who grow up in unfavorable socio-economic conditions or in a dysfunctional family that does not provide enough of the necessary stimuli. Delays in the development of such children can be the basis of their lifelong emotional and intellectual disability. However, we know that even the development of such children does not have to be disrupted if they manage to find long-term support in an adult whom they trust and with whom they can identify. This important role can be fulfilled, for example, by one of the grandparents or a teacher at school.
Today, we perceive the development of the human individual very comprehensively. We believe that it is the result of the interplay of innate talents - especially temperament and cognitive abilities, and the influence of the environment. If the development is not disturbed by a serious illness or other unfavorable circumstances, both of these components will be applied equally in the development of the personality.
Summary: Opinions on the share of innate, hereditary talents and the share of the influence of the environment on the development of the child's emotional and intellectual abilities have developed in the past. Freud considered the influence of the environment to be decisive. Piaget used the new knowledge about brain development and considered the degree of maturity of the brain tissue to be the most important for the development of the child's mental world. Today, opinions prevail that the development of the human individual is the result of the interplay of innate talents and educational influences from the environment.
Embryo development
A child's development is a continuous process. For practical reasons, they are divided into time-limited sections, which are characterized by a certain degree of physical, mental and social maturity.
The individual development periods are listed in Table 1. The relevant following chapters discuss them in detail.
| Pregnancy week | Developmental stage |
|---|---|
| 1 | Fertilization and nesting of eggs. Beginning of embryo development. |
| 2 | The embryo has two layers of cells. |
| 3 | The first missed moons at the mother. The embryo has three layers of cells. |
| 4 | The embryo already has a human shape. His nerve tube is closing. It forms the basis of future limbs. The embryo measures 4-5 mm. |
| 5 | The original mouth and the bases of the fingers are formed. |
| 6 | The primary nose and palate form. The embryo measures 21-23 mm. |
| 7 | It forms the basis of the eyelids. |
| 8 | There are distinct gonads - ovaries or testicles. |
| 9 | The fetal period (period of fetal development) begins. Length 5 cm, weight 8 g. |
| 10 | The external genitalia are clearly evolving. |
| 20 | Weight 460 g, length 19 cm. |
| 25 | The third trimester begins. Weight 900 g, length 25 cm. |
| 28 | The fetus has open eyes. Tilts the header down. It weighs 1300 g. |
| 38 - 41 | Usual date of birth. |
The time spent in the mother's uterus (intrauterine period) is the most dynamic developmental period in human life. Within 280 days (nine calendar months), a single fertilized germ cell develops into a perfect human fetus that is capable of independent existence immediately after birth. There will never be so many groundbreaking events in such a short time.
We left the newly formed human life in the first chapter when the fertilized egg began to divide and gradually became more and more cells, all equipped with the same set of 23 pairs of chromosomes. On the sixth day after conception, the human embryo (embryo) begins to nest in the uterus. At that time, the embryo is a spherical cluster of cells with an inner cavity. On the fourteenth day, it already has two separate germ layers of cells. At that time, the nesting of the fetus in the uterus is successfully completed and the placenta begins to develop, which will mediate metabolism between the fetus and mother throughout the intrauterine life. In the third week, another, third layer of embryonic cells and the base of the neural tube, the precursor of the later brain and spinal cord, are formed. The first blood vessels appear and the heart begins to work.
Between the fourth and eighth weeks of its development, the embryo gradually acquires the form of a small human. The base of the arms and legs, muscles, vertebrae, upper and lower jaws, palate, ears and other parts of the head and neck appear. The base of the eye lens can be recognized where the eyes will later be. The brain grows fastest. By the eighth week, the embryo has already formed the basis of all future organs of the human body. The average large embryo at the turn of the 8th and 9th week, when we begin to call it a fetus, weighs 9 grams and measures 5 centimeters.
Summary: The period of development between conception and the end of the eighth week of intrauterine life is called the embryonic period (embryo = embryo). During this time, the embryo nests in the uterus and gradually forms the basis of all its organs. At eight weeks the embryo measures 5 centimeters and it is possible to clearly identify the base of the arms and legs, muscles, vertebrae, upper and lower jaws, palate, ears and eye lenses. The brain grows very fast, the heart works and the blood circulation works.
Fetal development
The period of fetal development (fetal period) is called the period from the beginning of the 9th week of intrauterine life to birth. From the beginning of fetal development, the individual parts of the fetal body enlarge, their number of cells grows and their appearance is completed. At 10 weeks, the fetus already has an unmistakably human face. At the same time, the final form of the digestive system is being completed. In 12 weeks, the development of the external genitalia is completed. The lungs begin to develop. By the 24th week, the development of the fetus' lungs will progress so much that in the case of premature birth, they can begin to breathe, even if only with the support of devices.
In length, the fetus grows relatively fastest between the 4th and 6th month of pregnancy. However, fetal weight does not increase significantly until the last three intrauterine months, starting from the 25th week of pregnancy. In these three months, the weight will triple. At that time, the fetus's body builds up reserves of protein, adipose tissue, iron and calcium for the period after birth. At the very end of intrauterine life and the first six months after birth, boys grow faster than girls because they temporarily produce a certain amount of male sex hormones at this time. Only then does the production of sex hormones cease and resume to the threshold of adolescence.
The weight of the fetus before birth affects the length of pregnancy, nutritional status and health status of the mother. Further weight gain inside the uterus is already difficult due to the cramped intrauterine space.
Summary: The period of fetal development (fetal period) begins with the 9th week of intrauterine life and ends with birth. Already in the first weeks of the fetal period, the fetus acquires a human face. The development of the external genitalia ends and the lungs begin to develop. The fetus grows the fastest in length in the middle of pregnancy, but the weight of the fetus increases significantly, especially in the final three months, when the fetus builds up nutrient reserves for the period after birth.
Life manifestations of the fetus
The fetus begins to become active very soon during intrauterine development.
Minor muscle contractions appear around the 8th developmental week, ie at the very end of the embryonic period. At 13 and 14 weeks, the fetus begins to swallow amniotic fluid and indicates respiratory movements. Gradually, they learn to respond by moving to touch. By the 17th week, a touch in the palm of your hand will evoke a grip on the hand. This "grip reflex" will be fully developed by the 27th week. At week 26, the fetus opens its eyes for the first time.
In the middle of pregnancy, around the 20th week, the mother begins to realize the movements of the fetus in the womb. Each fetus has its own physical activity. Experienced mothers may notice the differences themselves, and the different agility of the individual fetuses can be well illustrated even during the ultrasound examination. When mom drinks coffee, the fetus begins to move more. It probably reacts to the effect of caffeine.
An unexpected new sound stimulates the fetus to lively movements. If the same sound is repeated more than once, the physical activity will weaken. This shows that the fetus can get used to a certain sound and that it can already learn: It learns to respond to stimuli from the external environment.
Summary: The fetus begins to move very soon. The first muscle internships in the 8th week are followed in the 13th-14th swallowing and breathing movements. Between 17.-27. the grip of the palms develops within a week. From mid-pregnancy the mother feels the movements of the fetus. Each fetus has its own distinctive physical activity. The fetus is already able to learn: It responds to the new sound with a lively movement, if the sound repeats, the movement response weakens.
Birth
During intrauterine life, the little man takes all the necessary nutrients and oxygen through the placenta from his mother. At birth, the placenta loses its function and the newborn begins to adapt to a new, independent life.
The first breath after birth of the air lungs and the baby from this time ensures the supply of oxygen to the body by breathing. His blood circulation adapts to this. The heart directs the main blood flow to the lungs, where the blood is enriched with oxygen. Oxygenated blood then flows throughout the body and supplies oxygen to all its parts.
In the first hours after birth, the newborn begins to eat orally for the first time. He is equipped with a system of reflexes, automatic reactions that will make it easier for him to get food. The most important are the search reflex and the suction reflex. When a little man feels a touch on his face, he turns his head towards the point of contact thanks to a search reflex, because he expects his mother's nipple, the source of food, there. She tries to hug her nipple with her lips. By sucking reflex, creating a vacuum in the oral cavity, after finding the nipple, she begins to suck breast milk.
There may not be enough food in the first days. My mother's breasts are only gradually beginning to form an abundance of ripe breast milk. The mother is also just learning to breastfeed if she has her first baby, and at the same time she is learning to suckle more and more effectively. Therefore, for the first days after birth, the little man created fat reserves in the last three months of pregnancy, which help him to overcome this period. Therefore, even after birth, they usually lose part (up to a tenth) of their birth weight. With sufficient nutrition, he usually catches up with this loss by the 10th to 14th day of life. In the first month, an average of 30 grams is added each day, although this weight gain can fluctuate significantly day by day.
In addition to new functions of respiration, blood circulation and digestive system, the kidneys are also newly applied after birth. While in intrauterine life, fetal blood has been purified from metabolic waste products in the placenta, the kidneys take on this function after birth. Like other organs, the kidneys are well prepared for their new function at birth.
Summary: With the first breath after birth, the newborn's lungs play a vital role - supplying the body with oxygen. The function of the blood circulation changes, which begins to distribute oxygenated blood from the lungs to the whole body. The baby begins to eat by mouth. The search and suction reflex helps him to obtain food. Weight loss of up to a tenth of birth weight after birth is natural, but the newborn usually compensates for it by two weeks of age.
Newborn and the surrounding world
Every newborn baby is born with a certain temperament, with a different degree of adaptability and a tendency to the typical form of reactions to the surrounding stimuli. Some little people are calm, balanced by nature, others exciting, more irritating. This does not mean that one behavior is better than another. This means that every newborn is already a unique personality.
Parents react to the behavior of their newborn in a certain way. It is their reactions to the child's life manifestations that stimulate his further development in the first days and weeks of life.
The newborn has surprisingly well-developed some sensory abilities that have only recently been recognized in more detail. From the first days of his life, they help him to perceive the world around him, to orient himself in it and to learn to respond to it.
From the senses, the newborn's hearing is surprisingly well developed. A newborn baby recognizes the sound of human speech well. She pays attention when she hears a woman's voice with a higher frequency. He expects the food source to be approaching. On the contrary, a deeper male voice with lower tones rather calms him down. A loud scream with a high frequency will cause him anxiety just like an adult. During the first weeks of life, the newborn learns to distinguish the voice of the mother (the person who brings him food) from other female voices.
A newborn baby can use smell well. Smell best helps him orient himself in the environment. The newborn turns away from unpleasant odors, while pleasant smells attract him. Already a week after birth, she recognizes the smell of the mother's nipple. He was found to perceive the smell of the mother, not just the smell of breast milk.
Even taste has its function from birth. Even a small person has even more taste buds than an adult. The newborn prefers a sweet taste and avoids bitter or otherwise unpleasant tastes.
Eyesight gradually improves after birth. The retinal light-emitting cells are already mature at birth, but the lens that is needed to focus the image on the retina is not yet perfectly mobile. Thus, visual acuity is low at birth. Within six months, visual acuity develops by approaching an adult. Within two months after birth, the baby gradually learns to perceive the object in its field of vision. Infants prefer to look at the human face rather than geometric shapes and prefer curves and bright and contrasting colors. Squinting is common in the newborn and is not a sign of the disorder. Within three months of age, squinting usually disappears. If it persists, it is advisable to examine the eyesight after six months.
Summary: A newborn is born with a certain temperament and with varying degrees of adaptability. His behavior provokes reactions from his parents, which further support his development. The newborn has well-developed hearing, smell and taste. Later, visual acuity also improves. These sensory abilities help him to orientate in the environment and thanks to them he gradually learns to react differently to different stimuli.
Life manifestations in the first months of life
In the first weeks of life, a small person cries very often and for a very long time. The time he spends crying is usually the longest in six weeks of life. At that time, he cries up to three hours a day. Crying is the main way in which he draws attention to himself and expresses both pleasant and unpleasant feelings. It can be a reaction to such diverse situations as hunger, wet diapers, fear or fatigue from an excess of stimuli. Sometimes the cause of crying cannot be determined. Around three months of age, crying usually decreases significantly. The child spends less than an hour a day crying. Gradually, they learned to react in a more diverse way - smiling, touching hands or fingering fingers.
In the first weeks of life, a child's crying may worry parents, especially in more irritating children. Parents of very sensitive children who need a little stimulus to make them cry need to understand their little one's original temperament and need to know that further excessive stimulation will strengthen his crying. It's a great art. Many parents tend to create more and more stimuli for their children when they cry. The baby can be calmed by a pacifier, rocking, calm silent singing or behavior in his arms. It is important to keep in mind that crying is only limited to a short period of the child's life and that after the third month, these symptoms gradually calm down.
The rhythm of sleep and wakefulness is initially random, irregular. Due to the gradual maturation of the brain tissue, over time, ever longer periods of uninterrupted sleep stabilize, alternating with longer waking times. The child gradually learns this rhythm. If his parents make many contacts with him during the day and stimulate him, they will learn to sleep more at night. Around two months of age, most infants wake up two to three times at night for a short period of time and are required to be fed. But some can sleep uninterrupted for up to six hours. The total sleep time gradually decreases during development, as shown in the table.
| age | hours of sleep total | of which during the day | |
|---|---|---|---|
| 1 week | 16 | 8 | |
| 1 month | 15 | 7 | |
| 3 months | 15 | 5 | |
| 6 months | 14 | 4 | |
| 12 months | 14 | 3 | |
| 2 years | 13 | 2 | |
| 3 years | 12 | 1 | |
| 5 let | 11 | - | |
| 9 let | 10 | - | |
| 14 let | 9 | - | |
| 18 let | 8 | - |
Summary: In the first weeks and months of life, crying is the main way a young person responds to a variety of stimuli - hunger, wet diapers, fear or fatigue from excessive stimuli. She cries around the age of three months as the baby learns to react in a more diverse way. The total required daily sleep time gradually decreases from almost 17 hours after birth to 14 days per year of age and to 8 hours on the threshold of adulthood. The little baby gradually learns the regular rhythm of sleep at night and waking up during the day. It helps him if his parents make extensive contact with him during the day.
Exploring the world in the first year
Freud, Erikson a Piaget represent the basic three developmental theories, which each from their point of view assess the individual developmental periods of a person's life. Each of the theories brings a new, interesting developmental perspective.
Piaget called the first two years of life a sensorimotor period. He tried to express a straightforward relationship between the stimulus from the environment, which the child perceives through his senses (sensors), and his movement response (-motor). The little man is gradually learning to combine sensory perception from the environment with a suitable movement reaction in an increasingly ingenious way. The youngest infants are still based on simple, relatively stereotypical reactions (an example is the suction reflex). However, they constantly supplement and improve them thanks to the accumulated experience, which increases with the development of other sensory abilities, especially sight and touch.
In the first year of life, the child perceives only his immediate surroundings: the persons and objects he sees and touches. The little man can watch the movement of the object in his field of vision. In the first half of his life, however, the subject ceases to exist as soon as he leaves the field of vision. Between 9 and 12 months of age, he begins to understand the permanence of objects - the fact that objects exist even when they are not visible. He first tests his idea of the permanence of objects on the example of his mother, who is the most emotionally important of all persons and objects.
In the second year of life, the ability to manipulate objects with tools then gradually develops. At the same time, the child first imitates, later he tests himself and learns by trial and error.
According to joy the first year of life is called the oral stage (oral = oral), because the child satisfies his important needs through the mouth. He sucks food from the breast or a bottle, soothes by squeezing his thumb or pacifier.
The first year of life is a time of complete intermingling of a mother and her child. In fact, there is almost no boundary between them. The mother satisfies all the needs of the child and future lasting bonds are formed between the two. Not only the mother, but both parents learn to perceive and recognize the expressions of their child, by which she expresses her needs, and to satisfy him. Erickson talks about the phase of primary trust or distrust that the child gains during this period thanks to his parents. Much of this initial trust or distrust carries with it for the rest of your life.
The first social game in which the parents alternately show and hide the child and the child alternately watches them and then turns to the other side is typical of the second quarter of life. It brings joy and pleasure to both - the child and the parents. It is also the first attempt at imitation, which is needed for the later development of skills and social behavior. The child begins to understand more complicated games, such as the game of hide and seek, later - usually around the 9th month.
Between the ages of eight and nine, fear of separation and strangers begins to emerge. It is a natural consequence of brain maturation. Thanks to him, the child is able to recall previous experiences and be able to incorporate new observations into them. It also recognizes events that are only partially similar to previous experiences. However, new situations evoke his uncertainty and gradually his fears and anxieties. This is already a relatively complicated brain function, which the child was not able to do until then.
When in contact with an unknown person, the child first examines his face and remembers whether he has seen it. If he finds that the face is unknown, he gets scared and can react crying. The fear of separation from the mother arises when the baby begins to be able to remember the presence of the mother, even if he does not have it within reach. He finds out that something is wrong, he becomes uncertain, he starts to worry and he reacts by crying.
This behavior begins in the child around the 8th month, peaks around the 15th month and naturally disappears around the age of two, as further brain maturation facilitates the development of new behaviors. Parents can "fool" the child: If he places a picture of his mother near him so that the child can see her face in her absence, the child can calm down.
Sourhn: A small infant first reacts relatively stereotypically. With the growth of new knowledge, which is also facilitated by the development of sight and touch, new stimuli are increasing and the way of reaction is more and more diverse. At first, the child perceives only objects and persons he sees or touches, but between the 9th and 12th month he already understands their permanence. During the first simple social games with parents, the child learns to imitate. Between eight and nine months of age, fear of separation and fear of strangers appear. It is caused by further maturation of the brain, which already allows for more complicated thought processes.
Growth in the first years of life
Birth weight and birth length depend on the length of pregnancy, the nutritional status of the fetus and the health of the mother. The height of her parents has little effect on her.
In the second half of the first year of life, the child's growth begins to be influenced more by genetic talents, derived primarily from the height of the parents, much less from the height of the grandparents. Between birth and the end of the second year, the length or height of a child can change significantly in both directions compared to other children of the same age. At the birth of a minor, who has higher parents, it usually grows relatively fast and in the second year of life it is already included in the higher band, which corresponds to the parental height. Conversely, a relative downward shift in height can occur in large babies whose parents are smaller. Such children can grow slower or less gain weight, so that in the second year of life their height corresponds to the talent inherited from their parents. This change can sometimes worry parents and lead to misconceptions about the child's poor well-being.
On their first birthday, the baby weighs about three times more than at birth and multiplies its length by an average of 1 time. After the second birthday, the growth rate will gradually stabilize at the values typical of middle childhood - the child will then gain 2-3 kg per year and grow by 5 - 7,5 cm. Until the beginning of adolescence, children then maintain a permanent place among their peers in terms of their height. It also largely determines their adult height.
Boys usually reach their future adult height around the age of two, girls in a year and a half.
Summary: Length and weight at birth say little about a child's future height. It is only after half a year of life that the aptitude for body height inherited from the parents becomes more popular. By the age of two, the child is gradually placed in his or her height range, which he or she then maintains throughout his or her childhood until the beginning of adolescence and which also largely determines his or her adult height.
Adult height prediction
Parents often ask how big their child will grow up. You can try to calculate for yourself what talent for future adult height you have given to your child.
This calculation is based on the fact that the difference in average height between adult men and women is 13 cm. A parent of the same sex gives the child a talent that corresponds to his own height, a parent of the opposite sex presents a talent increased by 13 cm (mothers to sons) or reduced by 13 cm (fathers to daughters). The view persists that the average height of children increases with each passing generation and that "children outgrow their parents". This fact was very noticeable in the first half of the twentieth century. However, thanks to sufficient nutrition and suppression of a number of serious childhood diseases, the generation of today's parents has already reached almost its optimal height, which cannot increase in the next generation.
So how do we calculate what aptitude for body height we have given our child? To the body height of a parent of the same sex, we add the height of the other parent increased (for boys) or decreased (for girls) by 13 cm and divide the sum by two. We get our child's most likely adult height. If we add 8,5 cm to this height and subtract the same number, the range to which our child grows with a probability of 95% is created.
Example: Paul's father measures 180 cm, his mother 158 cm. They are afraid that their son will not be too small for his mother. They calculate its probable height as follows:
| 180 + (158 + 13) | = | 351 |
| 351:2 | = | 175,5 |
| 175,5 + 8,5 | = | 184 |
| 175,5 - 8,5 | = | 167 |
The most likely adult height of the son will be 175,5 cm. It is 95% likely to grow to a height between 167 and 184 cm. Given the average height of adult men, which is around 178 cm, there are no concerns about its height.
The example also shows that the calculation is reliable, but it does not give a very accurate result. That's why we don't have to settle for it. In the next part of this chapter, we will learn to use percentile graphs, which will allow us to predict our child's adult height more accurately.
Percentile graphs delimit the usual body height ranges from birth to adulthood and are the result of measurements by thousands of children of all ages. Due to the slightly different growth patterns of boys and girls, they are prepared for each sex separately. You can find the percentage graph of body height in your child's "Health and Vaccination Card".
The horizontal axis (oxa "x") of the percentile graph represents age in years; vertical axis ("y" axis) body height in centimeters. The core of the percentile graph is the middle bold curve, called the 50th percentile. It shows the growth of a child with a medium height in individual years. Half of children of the same age are larger and half smaller.
This middle curve is surrounded at the bottom and top by parallel curves, which (from top to bottom) mark the 97th, 90th, 75th, 25th, 10th and 3rd percentiles. The percentile number expresses what percentage of children have a lower body height than the relevant curve. The area between the 25th and 75th percentiles is called the mid-height band. That includes half of all children.
Children with a height below the 3rd percentile are small, but even so, 3% of children grow in this zone. If there were 33 children in a school class, then one of them should naturally be less than the 3rd percentile. Likewise, in every school class of 33 children, one child should be above the 97th percentile.
Among children whose height deviates from the zone between the 3rd and 97th percentiles, most children are healthy, but in some of them their less usual body height may already be a sign of a health disorder. In this case, growth should be qualified by a pediatrician.
The percentile chart will therefore help parents compare their child's height with other children of the same age.
Example: Pavel is eight and a half years old, measures 124 cm and is the smallest in the class. His parents are worried about his growth, as some classmates measure more than 140 cm.
In the percentile chart of boys, we find that at the age of 8, the average height of boys is 133 cm (50th percentile). The height of 124 cm lies on the 10th percentile, so every tenth boy of the same age is smaller than Pavel. Of course, it can happen that all the boys in the class are bigger. The tallest boys can measure 143 cm (97th percentile) or even more.
The second use of the percentile graph is to estimate future adult body height. For such an estimate, we can use a child's height from about two to ten (for girls) or up to eleven (for boys). We already know that within two years a child's height is still subject to fluctuations - and so it is during adolescence.
From the point that marks the current height of the child, we extend the imaginary curve parallel to the nearest percentile curve to the right edge of the graph until the age of 18. The point where this imaginary curve intersects the right edge of the graph indicates the probable adult height of the child.
Example: Paul's parents are not satisfied with finding out that every tenth boy of the same age is smaller. They are still afraid that Paul will remain small. They want to know an estimate of his adult height.
If Pavel measures 8 cm at the age of 124, his height lies at the 10th percentile. We follow the 10th percentile curve to the right. The right edge of the graph (the vertical axis, which corresponds to 18 years of age) intersects this curve at a height of 170-171 cm. This is most likely Paul's adult height.
A third way to use the percentile chart is to monitor growth over time. A healthy child usually does not change his height band in the percentile chart between the second birthday and the onset of puberty. Even growth along a certain graph curve is the best proof of a child's long-term good health. It makes sense to repeat the measurement no more than half a year, because the growth rate may be subject to slight seasonal fluctuations. However, especially for the purpose of long-term growth monitoring, it is necessary to pay attention to the accuracy of the measurement when determining the height, so that there is no unnecessary doubt about the growth rate of the child.
Summary: To monitor a child's growth, parents can use percentile charts to help compare their child's height to their peers' height and to monitor long-term growth. The adult height of the child can be estimated both by calculation from the height of the parents (less accurately) and by using a percentile graph by stretching the imaginary curve parallel to the graph curves from the current child height to the right edge of the graph (more precisely, but only for children between two and ten or eleven years of age). ).
Brain development
The brain is the most complex and richly structured organ in the human body. Thanks to the brain, which is the most perfectly developed in humans of all animal species, our way of life has thus significantly moved away from our closest relatives, apes, and allowed us to create a specifically human abstract world, best seen in spoken and written words.
The fully developed human brain contains about 100 billion interconnected brain cells. The majority of brain growth takes place during the first three months of intrauterine life, and at birth the number of brain cells is finite. However, the brain continues to grow somewhat and, in particular, matures, which means that the brain cells gradually improve their arrangement and thus their function. The newborn's brain has already reached three-quarters of its future adult size, and the head, which reflects the size of the brain, makes up a quarter of the body's length. This ratio changes significantly during further growth and development, and at the age of 25 the head is only one-eighth of body height. So after birth, the rest of the body grows by more knowledge than the head, that is, the brain. It is certainly a well-known experience for parents that a child grows out of trousers rather than hats.
After the second year of age, the circumference of the head increases only slightly, by a maximum of 2 cm per year. At 7 years of age, brain growth is 90% complete, and at 10 years of age, the brain reaches adult brain weight.
An important part of brain maturation after birth takes place during the first four months of life. Thanks to him, the reflexes typical of the newborn period gradually disappear, the child is more and more alert and responds more to the surroundings. The infant is already trying to grab objects, smiles and laughs out loud, expects to get the food he has in sight, and gradually begins to sit with support.
The maturation and development of the brain is very closely followed by the development of the child's psyche and mental abilities, as well as his dexterity, the ability of motor coordination (so-called fine motor skills). The gradual development of dexterity can be well observed in the first year of life, for example, in the way a child grasps an object with his hand. The ability to grip usually appears at 3-4 months of age. This new skill brings a lot of joy and pleasure to the child. First, he begins to grasp objects with his entire palm. The thumb, as part of the palm, engages the grip later, in the fifth month. In the seventh month, he begins to help the baby grasp some objects, such as cubes, his thumb turned against the other fingers. Up to 9 months of age, a child can also use a fine tick grip to grip crumbs or small balls. As in all other skills, it is true that each child is a separate individual and his development may differ slightly from the data. We mention average data obtained during the evaluation of large groups of children.
The overall physical development (so-called gross motor skills) is of great importance for the child to discover the surroundings. The baby usually begins to sit independently between the 6th and 8th month. From now on, he can observe what is happening around him without restriction, and his horizon continues to expand. He starts walking around the age of one year (with a range in healthy children between 9 and 17 months of age). Thanks to independent walking, the child can enter the second year of life with straight feet, the main purpose of which is to gradually gain independence and discover the world independently.
Summary: The brain is the most complex and perfect organ in the human body. A substantial part of brain development takes place before birth, even though the brain matures for some time after birth. The maturation of the brain is followed by the gradual development of the child's psyche and mental abilities, as well as his movement skills in the field of fine and gross motor skills. Movement skills help to further develop the psyche, because the child grasps and inspects the objects, then sitting significantly expands his field of vision and later, thanks to independent walking, the child can begin to discover the world on his own.
The second year of life
Independent walking brings an important turning point in a child's life. The child can start to move away from the mother and explore the surroundings. The first timid steps to independence begin. The mother continues to be a strong point in the uncertain world for the child, and the child often returns to her to make sure she is present. However, he begins to understand that the environment belongs to his world and in this context he begins to realize himself.
This period can bring with it the first serious educational problems typical of the second year of life: At this age, every child tries to form his or her own idea of what he or she can conquer from his or her surroundings, but lacks experience. He sometimes gets into dangerous situations. Some serious child injuries, such as scalds, are typical because a child may drop a container with hot contents during their research. Some parents restrict the child's research activities with a number of prohibitions, orders, or even punishments, in order to prevent such dangers. However, they do not realize that the child is currently going through a fragile period of his personality development and the suppression of his independence may disrupt this development. It is more appropriate if the parents do not prevent their child from increasing independence, but take measures that support the child's research efforts and at the same time reduce the risk of injuries. Containers with hot contents are placed on the rear burners of the stove, entry to the stairs is prevented by the installation of a suitable enclosure and the like. Some commercially available aids sold by IKEA, for example, can be used to prevent toddlers from making excessive research efforts after easy installation.
Along with self-perception, the child begins to understand the feelings of other people. He develops empathy, the ability to empathize with another person. He wants to please someone who is sad and shows participation if the other person has hurt himself. He realizes how the second child feels when he hits. This helps him control his own aggressive behavior because he tries not to hurt the other. He gradually learns to perceive what is right and what is wrong and understands better what his parents expect from him. When he does something "bad", he shows anxiety. When he succeeds, he is happy. The role of parents is to help the child to define the terms "correct" and "incorrect" in a reasonable way.
Even this rapid development of cognitive, emotional and motor skills is due to the maturation of the brain tissue. This is also a prerequisite for practicing cleanliness, one of the main tasks of a child at this stage of development. Toddlers already perceive a full rectum and bladder and are able to control the activity of the anal sphincter. When they are positively motivated, they enjoy their success in keeping them clean. However, cleanliness training should not be rushed. Each child's ability to consciously control sphincters at a slightly different age matures. Well-known child psychologist prof. Matějček warns parents against dropping out of the potty too early, which can sometimes have practical reasons (consumption of diapers decreases and childcare will be easier), sometimes prestigious (comparison of educational success with other mothers of children of the same age).
When practicing cleanliness, every child needs the help and support of their parents. When parents start punishing a child for failure, cleanliness problems can be the subject of a long-term struggle between the parents and the child, and in some cases can form the basis of later emptying difficulties.
Freud he calls this period of the child's development the anal stage (anus = rectum), because the practice of purity is the main task that the child should master perfectly. However, it is also an expression of practicing social behavior in a broader sense. At this age, the child should learn, among other things, to control his impulsive and aggressive behavior and should know what kind of behavior is socially appropriate. Freud attributed the practice of purity to the influence of the development of necessary qualities such as diligence and conscientiousness. However, these characteristics are probably more a manifestation of a certain stage of development, thanks to which the child also learns to maintain cleanliness.
Summary: Independent walking in the second year of life is the beginning of the development of the child's independence and independence. The child tries to explore what he can conquer from his surroundings. At the same time, they may be at risk of injuries that reasonable parents can adequately prevent, but they should not visibly hinder the child's research efforts. Thanks to the development of the brain, the child's emotional experiences deepen, the child perceives the terms "right" and "wrong" and has the prerequisites for practicing social behavior. With the right motivation, they will learn to keep clean.
Speech development
Communication with the outside world is important for a child from birth. The newborn and the infant make nonverbal contact with the person treating him, especially the mother. We talked about the methods of this communication in detail in the relevant chapters.
From the age of two months, this contact gradually begins to acquire a voice, as the child slowly learns to control his or her speech. The first vowel sounds ("e") that a baby begins to make at this age also inspire his mother to make a voice answer, and gradually a form of voice play develops between them, which brings joy and pleasure to both of them.
In the third quarter of life, the baby begins to chatter and repeat syllables ("dadadada"). It helps him to better control the small muscles of the oral cavity, which he is able to do due to the further maturation of the brain structures. The chatter phase culminates around the child's first birthday. At that time, however, most children start to feel the need to use individual words to describe people, objects and activities. He expresses his wishes and needs by pointing at objects at the same time. The number of words used with a specific meaning is slowly increasing. In a year and a half, the number of words used ("active dictionary") is different for each child, on average 20-50 words. The family can stimulate or hinder the development of their child's speech. If parents or siblings do not stimulate and overuse non-verbal means of communication, such as pointing, the development of the child's vocabulary will slow down. Speech development can also be adversely affected by recurrent otitis media with transient hearing loss. Intact hearing is therefore another condition for speech development. That is also why a child whose development of speech skills is significantly delayed should be professionally examined.
The ability to understand speech ("passive vocabulary") develops faster than the ability to express oneself. The child begins to understand the meaning of the first words as early as the 9th month. A month after the first birthday, he can understand 20-100 words. After 18 months of age, both active and passive vocabulary develop rapidly. Shortly before the second birthday, there is usually a significant leap in speech development: The child begins to compose words into simple verb sentences and spontaneously begins to describe his activity, often at the time he is performing it ("I'm going out."). He inserts prepositions into speech and begins to ask interrogative sentences with the words "why" and "what". He begins to realize time and begins to use the time factor in his speech. With this progress in expressive abilities, the child is directly concerned about richer contact with other people and about new and new information that helps him to get to know the world and orient himself in it. Its cognitive development gained a new significant impetus. The words used, which no longer only express specific persons and objects (verbs, prepositions, particles), also indicate that the child has acquired the ability to use speech in an abstract, symbolic sense.
Summary: Interpersonal communication, important from birth, acquires a voice from the age of two months. Thanks to better control of the speakers, the baby will gradually chatter and repeat syllables from the age of six. Around the first birthday, he feels the need to use the first concrete words. Both passive (understanding words) and active (self-expression) vocabulary then develop rapidly. Around two years later, he begins to put words into simple sentences, ask questions and use speech in an abstract sense.
Preschool years
Piaget calls the stage of development of two- to six-year-olds pre-operative. It begins at a time when speech has made it easier to create ideas in a symbolic sense. The child learns to manipulate the symbolic world. However, he still does not know how to separate reality from fantasy. He can therefore be afraid of his ideas and dreams. Parents who perceive their child's feelings with their experience and advice can help dispel his or her excessive fears.
Children's vision of the world is mostly egocentric. The child perceives the environment in relation to his wishes and needs. He does not clearly understand the relationship between cause and effect and tends to explain it egocentrically. For example, a child may perceive a parent's divorce in relation to his person: "Dad left us because I was angry." Or, "Dad left us because he didn't like me." He may also misinterpret the cause of the disease. He may perceive his sibling's illness as a result of a recent conflict or desire for a sibling to become ill. He may therefore suffer from guilt. It is up to the parents to realize this and explain to the child the true cause of these events.
A child at this age attributes human feelings to inanimate objects ("The car is glad to have a nice color."). He has the idea that people control all natural events. When asked why the sun sets, he answers, "She's going to her house." Or, "Someone's pushing him down."
Children's unrealistic thinking peaks between the ages of three and five, as symbolic thinking enriched by new experiences creates increasingly complex fantastic visions. Fantasy helps children to develop their sexual identity, to identify with their own life role and to grow emotionally. In their imagination, children test new life experiences, both in their imagination and in real play. At this age, the game can be based on imaginative ideas and can reflect the child's internal problems such as anxiety, insecurity in interpersonal relationships and repressed aggression. Children make up imaginary friends, but they often suffer from night terrors and are afraid of ghosts. Perceiving the content of a children's game will help adults to understand what is going on in their children's thinking and whether they need help, explanation or advice in a particular way.
In the company of other children, the child overcomes this phase more easily than if he is alone among the adults. The character of children's play in the team, such as kindergarten, is also gradually changing. Children who initially play "side by side" (parallel game) are starting to play more and more "together" (cooperative game).
Freud he calls the phase between three and six years of age the Oedipus phase, because the child has a strong connection to parents of the opposite sex. Children's imagination can focus on playing the adult with this parent. At the age of 6, Oedipus' manifestations begin to recede and long-term ties to same-sex parents strengthen.
Summary: Preschool children learn to manipulate the symbolic world, but they do not know how to separate reality from fantasy and can be afraid of their ideas and dreams. They perceive the environment mostly egocentric, in relation to their person. They often misunderstand the cause-and-effect relationship. If parents learn to recognize these manifestations of their still immature perception of the world, they can help their children overcome unnecessary fears, anxieties and remorse.
Preparation for school and first class: 5 - 7 years
Kindergarten attendance between the ages of 5 and 6 is considered an integral part of schooling in many countries. The child is much more mature for making contacts with his peers than before, during the period of parallel play. Staying in a group of children will strengthen its development towards independence. Separation from parents at this age is usually easily tolerated by the child, it does not bring him too many adverse feelings.
By this time, the brain had reached 90% of its adult weight. At about the age of 6, the last significant step in the reconstruction of the cerebral cortex takes place. Thanks to it, fine sensor-motor coordination (the relationship between sensory perception and gentle motor response) matures. It significantly helps to master school skills - both when working with a pencil and paper, ie when writing and drawing, as well as during physical education and sports.
Before the age of six, the child solves the task in a way typical of the pre-operative phase - he always focuses on mastering one specific problem. However, spatial imagination is already beginning to develop - at 5 years most children can estimate length, at 6 years weight estimation and at 8 years volume estimation.
After the age of 6, in the first grade, the child's main interest is mastering new school skills - recognizing numbers, letters and words, reading and writing them. Piaget refers to this period as the period of specific operations. The child began to be able to perform mental operations that contain more than one variable when solving a specific problem. He is able to sort objects, mark them with numbers and assess their properties, if they are specific objects from a known environment. In the first years, school education is primarily focused on such activities. Imaginary thinking recedes somewhat into the background and the child already understands the relationship between cause and effect. However, fantasies and imagination can persist in children's games.
Summary: Around 6 years ago, the last significant reconstruction of the cerebral cortex takes place, thanks to which sensor-motor coordination (the relationship between sensory perception and gentle motor response) is improved, which is needed for writing and drawing, as well as for physical education and sports. After starting school, the main interest of the child is to master specific school skills, for which he usually has all the prerequisites. Fantasy thinking is receding somewhat, but it may persist in the themes of the games.
Other school years: 7 - 11 years
The seven-year-old schoolboy has two main interests: To be successful in school and to gain a position in the team of peers.
School responsibilities are becoming more and more demanding and require concentration, constant attention and the ability to independently process increasingly complex information that comes in the form of spoken and written words. For the first time, intellectual performance becomes a crucial condition for success. In addition to intellect, school success is also determined by the child's emotional state, his ability to react and to maintain attention.
Some children who have a reduced ability to learn or learn more slowly may experience some school problems during this period. If a child is criticized by a teacher or parents for school failure, it can seriously demotivate him. If the child loses confidence in this way, other educational problems may follow. It is those children who show signs of school problems who need the most support and understanding in the family and at school.
Freud refers to these years as the latency period. In his opinion, the child does not have significant sexual or aggressive tendencies at this time and can devote most of his energy to school activities and friendships with classmates. In fact, already during this period, natural sexual elements gradually begin to appear, which have their basis in the incipient production of sex hormones in the adrenal glands. Aggressive traits appear in the boys' game, and girls and boys are gradually showing signs of interest in the opposite sex. Pre-adolescent sexuality is often fancy and focuses on movie stars and musical idols. Organized sports, club activities and similar controlled activities help to transform these natural aggressive and sexual tendencies in a socially acceptable way.
Summary: It is in the interest of the younger schoolboy to succeed in school and gain a position among his peers. Success in school is conditioned by intellectual performance, but also by emotional state and ability to concentrate. Children with a hint of school problems need the most support in the family and at school to prevent their demotivation. Due to the beginning of the production of sex hormones in the adrenal glands, natural aggressive and sexual elements appear already in this period, which can be suitably transformed during organized sports or club activities.
Pubertal growth uplift
After a quiet period of growth, which lasted throughout childhood and in which the child grew on average first around 7,5 cm, then around 5 cm per year, at the beginning of the second decade of life there is a growth stroke associated with adolescence (pubertal growth stroke). It starts on average at 10 years for girls and at 12 years for boys. During puberty, the growth rate gradually increases. At the very peak of adolescence, a girl grows on average 9 cm a year and a boy 10,3 cm.
First, the foot begins to grow rapidly - teens grow out of their shoes twice a year. The graphs in Figures 5 and 6 show gradual foot extensions. They show the mean, most common foot length at a certain age (mean fat curve, median) and the usual range (-2 SD corresponds to approximately 5th percentile, +2 SD to approximately 95th percentile - between the extreme curves has a foot length of about 90% of children). This chart can be used to plan the purchase of new shoes, but it is necessary to keep in mind that when your child's foot grows faster, they will temporarily grow faster than the mean values, so that their growth will definitely start to slow down definitively.
In the next phase of puberty, the lower limbs and later the torso grow rapidly. The face grows last. The most striking is the enlargement of the mandible, which increases by about a quarter between 12 and 20 years.
Puberty growth rate is the result of rapidly increasing production of sex hormones. Sex hormones significantly boost body growth, but even more significantly affect bone maturation. They naturally lead to the depletion and closure of the growth fissures of long bones - the main place from which the child and adolescents grow to heights. After closing the growth slits of the long bones, physical growth practically ends. This occurs in both sexes approximately five years after the onset of puberty.
Thus, boys experience their adolescent growth at least two years later than girls. Over the years, their lower limbs lengthen, less their torso. In addition, these two years of growth are the basis for later higher adult height in men than in women, by an average of 13 cm. Men now grow to a medium height of 179 cm, women to a medium height of 166 cm.
Due to the fact that adolescence begins in each individual at a slightly different age, the pubertal growth rate is differently timed for individual adolescents. However, the total duration of the growth trend is similar for all of them - around five years. The order of size in the school class at this age can temporarily change significantly. In particular, boys with a later onset of adolescence may suffer from a lower height for some time. However, they usually only suffer until they understand the laws of growth and development and learn that due to the later beginning of adolescence, they will grow even longer and at the end of their growth they will outgrow many of their earlier teenage classmates.
The opposite problem can be a problem for some early adolescent girls, who, due to early growth, tend to be concerned about excessive adult height. If they already have moons, their growth rate will decline rapidly and growth will end.
Summary: The pubertal growth rate begins on average at 10 years for girls and at 12 years for boys. At the peak of adolescence, a girl grows 9 cm a year, a boy 10,3 cm. However, due to sex hormones, growth then gradually ceases. In adulthood, men are on average 13 cm taller than women due to the later onset of adolescence. During adolescence, the order of individuals in the class changes temporarily according to size. The growth rate lasts around five years for all adolescents. Those who enter adolescence later will later experience their growth and grow longer and vice versa.
Adolescence
The development of the gonads, testicles in boys and ovaries in girls begins in the fetus as early as the 10th week of intrauterine life. After the 20th week of fetal development, the cerebral cortex begins to produce trigger hormones, gonadotropins, which act on the gonads and induce the maturation of germ cells in the ovaries.
Around birth and in the first months of life, the gonads produce certain amounts of sex hormones - estrogens in girls and testosterone in boys. Estrogens lead to breast swelling in some little girls. Then the activity of the gonads gradually dampens and their hormonal activity ceases. The rest period lasts until the beginning of adolescence.
The source of sex hormones in the body is not only the gonads, but also the adrenal glands, small glands that attach like a cap to both kidneys. During the resting period of childhood, the production of sex hormones in the adrenal glands is negligible.
Between the ages of 6 and 9, the production of sex hormones in the adrenal glands begins to awaken. These hormones contribute to the development of body odor because they stimulate the activity of the sweat and sebaceous glands. Gradually, they begin to contribute to the development of hair and the beginning of the growth boom. Especially for boys, they also lead to a focus on more aggressive ways of playing.
The gonads themselves enter function later. Gonadotropins begin to be produced in the cerebral cortex again and gradually stimulate the ovaries in girls and testicles in boys. While the adrenal hormones do not differ between the sexes, the gonads produce the sex-appropriate hormones and are responsible for pubertal development in the appropriate direction.
In boys, adolescence is controlled by the interplay of three groups of hormones: adrenal sex hormones, testosterone from the testes, and growth hormone from the brain, the production of which is enhanced in adolescence by testosterone. Before the age of 10, the testicles begin to grow slightly in the average boy. The first black hairs appear on the root of the penis. In the next phase of adolescence, the scrotum enlarges and its skin wrinkles, the penis enlarges, and in most boys (about 70%) there is swelling of the foundations of the mammary glands under the nipples (pubertal gynecomastia), which is a natural sign of adolescent adolescence. In the next stages of adolescence, the larynx grows and the voice deepens (voice mutation). The activity of the sebaceous and sweat glands also increases, which is why many boys are affected by skin pregnancy (acne). Growth hormone together with sex hormones strengthens growth. Muscle volume increases and the shoulders widen.
In girls, the first sign of adolescence is usually swelling of the mammary gland under the nipple, often at first one-sided. It occurs between the ages of 8 and 13, on average at the age of 11. It is a clear signal that the ovaries have already begun to produce female sex hormones - estrogens. At the same time, the growth boom is already noticeable and the first black hairs in the area of the birth can soon appear. Over the next 3-4 years, the hair in the typically female range gradually spreads and thickens, the size of the breasts and nipples increases, and the pelvis widens.
The first moons (menarche) usually come about two years after the beginning of breast development, in our country now on average at 13 years. Over the last century, the age at menarche has dropped significantly, probably due to improved nutritional status and the eradication of a number of serious childhood diseases. Malnutrition, low socio-economic levels, but also excessive sports training can delay the onset of months.
Initially, most menstrual cycles are not accompanied by egg release (ovulation), but pregnancy is not ruled out.
The pubertal growth rate peaks around the girls' menarche. After that, the growth rate decreases and the growth slits approach their closure. After the menarche, the girl will still grow 2 to 17 cm, 7 cm in diameter.
Summary: Between the ages of 6 and 9, the production of sex hormones in the adrenal glands begins in children of both sexes. They contribute to the development of body odor, the beginnings of hair and growth growth. The actual gonads, testicles or ovaries take office later, but they are already bringing a massive development of adolescence, including pubertal growth, development of secondary sexual characteristics and gradually fertility. The first months come in girls at an average age of 13, about two years after the onset of breast development.
Personality development in adolescence
Adolescence is a difficult period for every young person, during which the child gradually becomes an adult. Adolescents not only grow rapidly at this time and experience a change in their body proportions, but their cognitive and intellectual abilities also mature. It is not clear whether sex hormones are involved in these accompanying signs of adolescence.
All this leads the young person to a new phase of doubt about the current development of his personality. Again, he addresses his position among peers in a new sexually subdued context and goes through a new, deeper phase of striving for his own autonomy and independence.
Already around the age of 12 it starts with some adolescents according to Piaget ability of formal operations. When solving a certain problem, abstract thinking and an accurate perception of the cause-and-effect relationship are beginning to prevail. These teens are beginning to better understand the long-term consequences of their current actions. Their innate egocentrism is receding, and these young people are better able to understand other people's views.
However, not all adolescents have this phase going smoothly and harmoniously. Only a small proportion of adolescents mature into the stage of formal operations at this stage. For others, despite ongoing physical development, egocentric thinking may persist, with a tendency to simple solutions and an excessive focus on specific and physical aspects of social relationships. Some adolescents do not see the future consequences of their current actions and are unable to think abstractly. In an interview, they often respond in one word and cannot discuss the problem. Contact with them will be facilitated only by the choice of very specific, simple questions.
The development of abstract thinking is a gradual, complicated process. It begins with a look inside, introspection. Adolescents think about themselves, their own thoughts and actions, and may become proud of themselves because they can realize unprecedented relationships and contexts than in previous years of childhood, which they still remember well. This may be associated with a tendency to overlook others, especially adults. To do this, they use the newly developed ability to critically assess the thought processes of others.
In the next phase of adolescence, the moral dimension of thinking may appear in more mature young people. The moral laws of the family, group, and society are beginning to be more important in choosing their actions than the mere fear of punishment typical of years of childhood. The importance of the adopted rules of conduct is increasing and life, especially at school, is beginning to be subordinated to a large extent.
Those young people who find it difficult to find a job in a natural school group can look for another group, another environment where they could establish themselves. They can find alternative peer groups whose standards of conduct can reinforce anti-social behavior.
In late adolescence, most adult behavioral norms stabilize. Moral principles are reinforced, more permanent than group rules. The young person begins to take an active stand on what is good and what is bad and wants to solve problems on their own. Children's egocentrism definitely disappears and the real ability to empathize, empathize with others, is asserted. Thinking is flexible, flexible, which makes it easier to understand those who are different. Loss of impulsivity, adequate cooperation and perception of the long-term consequences of negotiations allow not only entry into high school and gradually a university with a freer style of study, but also definitive independence from parents and the beginning of a truly independent life combined with full responsibility for oneself and loved ones.
Summary: Adolescence is a difficult period. The adolescent himself re-evaluates his position among his peers in a new context and definitely strives for his independence and autonomy. Many adolescents are able to think abstractly with an accurate perception of the cause-and-effect relationship and with an awareness of the long-term consequences of current action. In the next phase of adolescence, the moral dimension of thinking appears and moral principles prevail in action. However, failure in the natural collective can lead to an escape into an alternative group whose norms of behavior can strengthen anti-social behavior.
Growth hormone treatment
Download full text: Growth hormone treatment [doc; 56,3 kB]
What is growth hormone?
Growth hormone is produced in the human body in the pituitary gland. The pituitary gland is a small round gland that is connected to the midbrain by a thin stalk. It is hidden deep in the cerebellum at the base of the skull.
From the brain, growth hormone passes into the bloodstream. Blood helps to distribute it throughout the body. In children, growth hormone stimulates bone growth in length and contributes to bone and dental maturation, in children and adults it also affects other important events - especially strengthens muscle mass, prevents excessive fat formation and storage, helps build bone strength and has a positive effect on the levels of some fats in the blood.
Thus, children need growth hormone to grow properly, but also adults, which it helps to live well.
Who needs to receive growth hormone?
Some children are unable to produce their growth hormone properly. Such a disorder may be congenital - or it may occur later in life, due to disruption of the cerebral cortex or the adjacent midbrain area.
Growth hormone deficient children grow little. Without treatment, they would remain very small in adulthood. Therapeutic administration of growth hormone can significantly increase their growth rate. If treatment is started early and lasts long enough, these children can grow to a completely normal adult height.
Not all low-growing children suffer from growth hormone deficiency. There can be many reasons for small stature. Therefore, it is first necessary to examine each slow-growing child in detail so that we can reliably identify the cause of the small stature.
Even some children who produce their own growth hormone can be helped by growth hormone therapy. These are children who need to have excess growth hormone for their sufficient growth. By adding growth hormone given as a medicine to their own growth hormone, we will help create this excess. This group of children includes girls with Turner syndrome, children with chronic renal failure and children with Prader-Willi syndrome.
In other children, the effects of growth hormone are still being tested - and in some we know that growth hormone unfortunately does not help them. Growth hormone is not a panacea that will allow everyone to grow as they wish. However, it is useful and necessary for those children who would not grow up properly without it and in whom we know it will be effective.
How is growth hormone produced?
Growth hormone is produced by so-called recombinant technology. The gene for human growth hormone was introduced into one cell, which can multiply quickly in the laboratory. Such a cell is then placed in a nutrient solution and begins to multiply. The number of cells grows and all these cells continuously produce human growth hormone, which they release into the surrounding solution. After a while, cell growth stops. At that time, the original nutrient solution already contained a large amount of growth hormone. The phase of removing cell wall residues from the solution and purifying the final product - growth hormone - takes place. In the end, additives are added to completely pure growth hormone, which prolongs its life. Growth hormone is filled into vials or pens.
This method makes it possible to produce growth hormone as needed, without restriction. We do not have to worry about its lack. At the same time, this production process ensures the production of completely pure human growth hormone without foreign matter.
How does growth hormone treatment work?
Growth hormone is a proteinaceous substance. Therefore, we cannot give it in the form of tablets, syrup or drops swallowed by mouth. In the digestive tract, digestive juices would break it down just as they would break down any other protein in the diet. It is therefore necessary to bypass the digestive system during treatment.
The only effective way to deliver growth hormone is through injection. Growth hormone is administered subcutaneously - in an easy and safe way that every parent can easily learn and that even older children can handle reliably on their own.
We probably recommend subcutaneous injections into the front of the thighs. This site is especially suitable for children and adolescents who inject growth hormone themselves, as the injection site is clearly visible during the injection and both hands are free to handle the injection. Suitable subcutaneous tissue is also in the upper outer quarters of the buttocks and in the upper outer parts of the arm.
Subcutaneous injection sites should be rotated. Repeated injections at the same site may cause swelling of the subcutaneous binder, from which the drug is then more difficult to absorb into the blood. When injecting into the front of the thighs, it is advisable to alternate the right and left leg every other day and create an imaginary midline - one week prick into the outer half of the thighs, the next week into the inner half of the thighs. We should move the injection site 2-3 cm every day. If we proceed correctly, we will not return to the original injection site until after 28 days, which is enough time to examine the subcutaneous tissue.
We inject growth hormone every night before bed. This best mimics the natural production of growth hormone in a healthy child. Healthy children produce growth hormone the most at night.
Growth hormone injections gradually become a natural part of daily evening "rituals" - the child brushes his teeth, washes himself, injects a growth hormone injection and goes to bed. Such a procedure will also help not to forget the growth hormone injection.
Growth hormone injections hardly hurt. Hundreds of children who receive it every day in the Czech Republic agree in this statement. Growth hormone is usually given with injection pens with a very thin needle that easily penetrates the skin. The pens also help to measure the correct dose accurately, as they are equipped with a reliable setting system. The injection can thus be given in a small volume, so that the unpleasant feeling of pressure when injecting the active substance into the subcutaneous tissue is almost eliminated.
The desire to grow properly is inherent in every child. Even young children will quickly understand that growth hormone injections are beneficial and helpful. Most children like to get injections and get along with them quickly.
Around the age of ten, children begin to be able to inject themselves. We should not force ourselves to do this, but it is appropriate to offer this option. However, children should be injected under parental supervision. Sometimes children tend to insert the needle only superficially - and the growth hormone comes out and disappears when the needle is pulled out. The needle should be fully inserted during the injection and, when pulled out, lightly push the pulp square to the injection site to prevent the solution from leaking out.
When do we stop growth hormone treatment?
Only long-term growth hormone treatment can best affect future adult height. Therefore, we usually administer growth hormone for many years, until the end of growth. We will recognize the appropriate moment to end the treatment according to the bone age determined from the X-ray of the wrist. Growth usually ends at bone age around 15 in girls and around 17 in boys. However, bone age may not be the same as calendar age.
More often than not, we decide to stop growth hormone treatment according to growth rate. If a teenager has grown less than 1 cm in six months, further growth can usually no longer be affected by growth hormone.
In children with growth hormone deficiency, after completing this treatment, we will check its own production in the brain pad. If a serious deficiency persists, it is useful to continue treatment into adulthood. At that time, growth hormone no longer affects height, but we use its natural beneficial effects on muscle, fat and bone tissue. Growth hormone thus contributes to a quality of life even in adulthood.
Treatment will no longer be continued in children who do not suffer from growth hormone deficiency, such as girls with Turner syndrome and children with chronic renal failure.
How do we store growth hormone?
Growth hormone is a relatively sensitive substance that can decompose into harmless but ineffective residues under the influence of heat. Therefore, it is necessary to store it in the refrigerator, in the lower compartment for storing vegetables. In this part of the refrigerator, the temperature is usually between + 2C and + 8C. However, growth hormone must not freeze.
One day of transport without refrigeration will not hurt the growth hormone - if we transport it home from our doctor, refrigeration is not necessary. Even in this case, he should not be exposed to excessive heat, as is often the case under the rear window of a car on hot days. Upon arrival home, we immediately store the growth hormone down in the refrigerator.
If we plan a longer trip, vacation or holiday, we will arrange in advance the possibility of storing growth hormone in the refrigerator. We will only take the amount of product that is really needed so that we do not transport it unnecessarily repeatedly.
Can there be complications during treatment?
Growth hormone treatment is safe. Tens of thousands of treated children rarely experienced health problems, which were usually related to the child's underlying disease and only marginally to the administration of growth hormone. Your doctor will tell you which indicators are appropriate for your child to monitor.
Your child will usually come for checkups every three months. By measuring the height and calculating the growth rate, your doctor will assess the effect of growth hormone, or adjust the dosage according to the child's weight. Laboratory samples will help assess the effectiveness and safety of treatment. If you yourself notice changes in the child's health in the meantime, do not hesitate to contact your care team by phone! Call even if you have technical problems with the pen. Although all growth hormone pens are extremely reliable, a technical problem cannot be completely ruled out.
Growth hormone treatment for illness, holidays, on the go…
Healthy children produce growth hormone continuously. Therefore, even the treatment of children with its deficiency should not be interrupted during the illness. Younger children in particular need it very much because of their illness, because it protects them from falling blood sugar levels, which they may otherwise face. This risk increases with temperature, anorexia or vomiting.
Other children who produce their own growth hormone properly are usually advised to discontinue treatment for a short period of time in the event of a more serious illness. On a day when the flu, chickenpox, pneumonia or other illness has exceeded the body temperature of 39 ° C, it is better to skip the injection so that we do not force the body to grow unnecessarily while fighting a more serious illness.
During the child's stay in the hospital, we will acquaint the well-caring staff with the operation of the growth hormone pen. We find that most healthcare professionals have not yet met with him. We will also draw attention to the possibility that an older child is able to inject himself / herself and that it is appropriate to use this option.
Discontinuing treatment during the holidays or on the go should be well considered. We achieve the best results in daily treatment. At the same time, however, we wish that the child is not excluded from interesting activities with his peers. If there is a risk of exclusion from school in nature, from a ski trip or from a boat trip for growth hormone treatment, a short-term interruption of treatment is possible. However, it should not exceed two weeks for the entire calendar year. If the child receives other medicines in tablets, we will not stop their administration!
When traveling, medicines belong in hand luggage. This protects us from complications in the event of theft or loss of luggage, which unfortunately cannot be ruled out when traveling by plane. In the case of customs control in more exotic countries, a doctor's confirmation in a foreign language that the child is being treated with growth hormone and that the transport of the drug across borders is necessary may be useful. Especially on hot days in the southern seas, we make sure to keep the time when growth hormone is not stored in the refrigerator to a minimum.
Turner syndrome
Authors:
Prof. MD Jan Lebl, CSc.
Doc. MUDr. Jirina Zapletalova, Ph.D.
Download full text: Turner syndrome [doc; 167,0 kB]
Introduction
This text deals with Turner syndrome, its causes and manifestations, and its treatment. It was created to provide information and instruction to all who are directly affected by Turner Syndrome - parents of girls with Turner Syndrome, older girls and women themselves, but also their doctors, who do not encounter Turner Syndrome often.
The text summarizes the findings on all known aspects of Turner syndrome. Girls and women who understand "their" Turner syndrome are known to be much more balanced and happier than those for whom their medical condition remains an incomprehensible secret. It is useful to familiarize Turner Syndrome with the wider family, teachers who have a girl with Turner Syndrome in their class and later, in upper school classes, as well as classmates and girlfriends of girls. The new information will also help them understand a certain difference in their good friend with Turner syndrome.
This text is intended for all of them.
1. How does Turner syndrome arise?
The human body is made up of many billions of individual cells. Every cell in our body has an assembly of 46 chromosomes in its cell nucleus. And each of these chromosomes carries a number of genes, carriers of genetic information. Genes are written on chromosomes in the form of a complex chemical compound called deoxyribonucleic acid (DNA). It is the genes that largely determine what a person will be. If he is big or small, blonde or dark-haired, brown-eyed or blue-eyed, what will be the features of his face, whether he will have musical or motor talent, and how developed will his spatial imagination, necessary for school success in mathematics or descriptive geometry. We could go on for a long time in this list of gene-borne traits. The genes stored in the chromosomes thus decisively determine both the physical characteristics of the human individual and his mental abilities.
At each cell division, the same set of 46 chromosomes is transferred to each emerging cell. Thus, a person has exactly the same set of chromosomes in each cell of his body that accompany him throughout his life.
44 of the 46 chromosomes are called autosomes. Their appearance is the same for women and men. The other two chromosomes are called heterochromosomes, or sex chromosomes. They decide whether the emerging little man will be a boy or a girl and grow up once into an adult man or an adult woman. Women have two female sex chromosomes, the "X" chromosomes. Therefore, their chromosome assembly (or karyotype) indicates 46, XX. In this formula, the number "46" denotes the total number of chromosomes and "XX" two female sex chromosomes X. Men, on the other hand, each have their own sex chromosome - one male "Y" and one female "X". Their set of chromosomes (karyotype) is described as 46, XY.
The future new man acquires his chromosomes just half from his mother and half from his father. The mother's egg carries 23 chromosomes in its nucleus, and one of them is the sex chromosome "X". Paternal sperm also carries 23 chromosomes. There is also one sex chromosome, in half of the cases the "X" chromosome, in the other half of the cases the "Y" chromosome. As a result, half of the girls and half of the boys are born. When a mother's egg is fertilized by paternal sperm, the two sets of chromosomes merge to form a definitive set of 46 chromosomes (23 pairs), which the new man obtains from his parents and which he will carry throughout his life. At this point, the gender of the future human individual will be decided. We see that the sex chromosome, brought by sperm, is decisive. An egg fertilized by sperm with the "X" chromosome turns into a girl, while fertilizing sperm with a "Y" chromosome results in a boy.
If an egg or sperm yields one chromosome less, or if one of the chromosomes is lost when they merge with each other, a set of 45 chromosomes is formed. If one sex chromosome is missing and only one "X" chromosome remains, the new human will have karyotype 45, X. And this is a typical karyotype for girls and women with Turner syndrome. In some cases, only part of one sex chromosome has been lost. Such girls have 46 chromosomes, but one of their X chromosomes is incomplete. An indication of the shape of the incomplete chromosome will then appear in their karyotype - eg 46, XrX, 46, XdelXq, 46, XiXq and the like. We refer to this condition as a "structural anomaly" or a deviating shape of the "X" chromosome. Girls with a structural X chromosome anomaly also have Turner syndrome.
Other girls or women with Turner syndrome have a "chromosomal mosaic" - a mixture of two or more different sets of chromosomes. In them, when the eggs and sperm fused, the set of chromosomes was perfect, but during one of the other cell divisions, one or part of the "X" chromosome was lost. These girls most often have a part of cells with karyotype 46, XX and another part with karyotype 45, X (45, X / 46, XX). The proportion of individual cell lines can be expressed in percentages. In practice, however, this is not important because the proportion of these cells in the blood, where the karyotype is usually examined, may not be the same as their proportion in important organs of the human body.
All of these groups of women and girls have Turner syndrome. Whether they have karyotype 45, X, a structural anomaly of the "X" chromosome or a chromosomal mosaic. Their problems are basically the same. We will therefore continue to talk about all of them together.

Giant. 1: Different karyotypes (chromosome assemblies) in Turner syndrome.
All three groups of girls and women have similar symptoms.
In particular, they have in common smaller stature and, for most, ovarian dysfunction.
We are still talking about women and girls. Men don't have Turner syndrome. If the X chromosome is lost in the chromosomal assembly and karyotype 45, Y is formed, the human embryo cannot develop further. There will be an early abortion. Human life without an "X" chromosome is not possible.
Exceptionally, in some girls, the male sex chromosome "Y" or a fraction thereof, usually in the form of a chromosomal mosaic, may be found in the karyotype in addition to the "X" chromosome. Most of these girls also have symptoms of Turner syndrome. However, we need to pay more attention to their gonads, as we talk about in the ovaries section.
How did Turner syndrome get its name?
In 1938, the American physician Herna Turner noticed that seven of his patients had some common characteristics: a small figure, a lack of pubertal development, a pterygium colli, a lower hairline at the back of the neck, and a limited ability to stretch the arms in the neck. elbow joints in a straight line ("cubiti valgi"). He published his observations in a well-known medical journal, and in his honor, this set of symptoms was referred to as "Turner's syndrome." Much later, in the 45s, when it was already possible to reliably examine the karyotype, this examination was actually performed on one of Henry Turner's former patients and karyotype XNUMX, X was found. In Germany, Turner syndrome is referred to as "Ullrich-Turner syndrome" in honor of the German physician Dr. Ullrich, who noticed for the first time a similar set of symptoms in a German girl. In Russia, for similar reasons, it is called "Turner-Shereshevsky syndrome".
Can Turner syndrome be prevented?
No one is to blame for Turner syndrome. The loss of the "X" chromosome or part of it is, as we know today, a random whim of nature. The onset of Turner syndrome does not depend on the mother's age or the health or habits of the parents. The mother's behavior during pregnancy with Turner syndrome is by no means related, because it was decided earlier, at the very beginning of the little man's development - when fertilizing an egg with sperm.
Turner syndrome does not occur more often in certain families. A family who already has a baby girl with Turner syndrome has no increased risk of developing it in the next pregnancy.
Therefore, the onset of Turner syndrome cannot be prevented.
How can Turner syndrome be detected?
Although in some girls the manifestations of Turner syndrome can be so conspicuous that the doctor already has an urgent suspicion during a routine examination, it is always necessary to examine the assembly of chromosomes in the cell nucleus for the definitive determination of Turner syndrome, karyotype.
The karyotype is most often examined in lymphocytes, one group of white blood cells. These can be easily obtained by taking blood. In the laboratory, these blood cells are allowed to grow - they form a "cell culture". At some stage in the growth of this cell culture, when the chromosomes are clearly visible, they are examined under a microscope and photographed. The chromosomes are cut out of the photograph, sorted into pairs, and found to be complete. In this way, at least thirty, but preferably more cells should be examined. The diagnosis of Turner syndrome is characterized by the absence or imperfect formation of one X chromosome in at least 5% of all cells examined. Usually, however, there are significantly more cells with an X chromosome disorder or all of them are affected.
In some cases, the result of the karyotype examination from lymphocytes may be questionable or still needs to be clarified. It may then be necessary to examine the karyotype of skin cells called fibroblasts. They are obtained by miniature collection of skin particles by skin biopsy.
The karyotype doesn't change during a person's lifetime. One reliable karyotype examination is sufficient for the diagnosis of Turner syndrome.
How common is Turner syndrome?
Turner syndrome affects one in 2000 to 2500 girls and women. In the Czech Republic, an average of 20-25 girls with Turner syndrome are born every year. In total, we have about 2000 women with Turner syndrome.
After finding out Turner syndrome, parents often think that they are alone with their problem, that they are abandoned in the middle of the parents of other, healthy girls. However, the relatively high incidence of Turner syndrome suggests that there are about 50 girls and women living in a city of 000 who have Turner syndrome themselves.
2. Turner's syndrome before birth
Turner syndrome can be detected during pregnancy. This is possible if the mother had a placenta sample (chorionic villi biopsy) or amniotic fluid sample (amniocentesis) or umbilical cord blood sample (cordocentesis) taken for genetic testing in the first half of her pregnancy for another reason. Turner syndrome may be an accidental finding in such an examination.
After such an examination, the parents have the right to decide for themselves whether they wish to terminate the pregnancy or continue it. Before making their decision, they should be familiar with Turner syndrome and realize that living with Turner syndrome has some complications, but that the vast majority of girls and women with Turner syndrome can live a rich and happy life.
Theoretically, it would be possible to detect Turner syndrome before birth in this way in all families. But it would mean subjecting all mothers to a demanding and burdensome examination, which is not possible in practice.
Exceptionally, Turner syndrome can be detected during pregnancy and by ultrasound. This harmless test is being performed today for all future mothers. However, it is unreliable for the detection of Turner syndrome.
3. Newborn baby girl with Turner syndrome
Girls with Turner syndrome tend to be born a little earlier and tend to have a slightly lower birth weight. However, this is not the rule - and even in this case, the date of delivery and birth weight usually do not deviate from the broader norm.
Swelling (lymphedema)
In some girls with Turner syndrome, swelling of the legs, especially the insteps, and hands (lymphedema) may be noticeable after birth. They arise because the fetus does not have enough small lymph vessels to drain fluid from the soft parts of the body back into the blood.
These swellings usually disappear within half a year or one and do not cause any problems. Only in exceptional cases do they last longer. However, after birth, they can bring doctors on the trail of Turner syndrome.
Skin fold on the neck (pterygium colli)
Another striking sign may be the skin lashes on the sides of the neck in some girls, which create the impression of a wide neck (pterygium colli). They have a similar cause: In intrauterine life, the tissue fluid settled in the neck area because it could not drain well. Pterygium colli does not cause any health problems. If the girl decides later in childhood or adolescence to surgically remove excess skin lashes for cosmetic reasons, it is possible to consult a specialized plastic surgery department.
Heart and blood vessels
Girls with Turner syndrome are more likely than other children to have a congenital heart or large blood vessel defect. Some heart defects appear in the first days of life, others are found out only during a targeted ultrasound examination of the heart. Every girl with Turner syndrome should have that. Almost all congenital heart defects can be successfully operated on today. If the baby has a good heart after birth, the parents no longer have to worry. Later in life, a heart defect will not arise.
In the case of finding a congenital heart defect or large blood vessels, girls with Turner syndrome are taken on by a heart disease specialist - a pediatric cardiologist.
Kidneys
The kidneys and urinary tract can also be somewhat different in Turner syndrome. The so-called "horseshoe-shaped kidney" is relatively common, when both kidneys at their lower poles are connected in the shape of a horseshoe.
These deviations only present exceptional difficulties. Nevertheless, every girl with Turner syndrome should undergo an ultrasound examination of the kidneys. Deviating kidney formation can, in some cases, make urine flow more difficult and promote a urinary tract infection. Regular investigation can detect and treat such complications in a timely manner.
Nails
Some girls with Turner syndrome have less usually shaped toenails, sometimes toes. They can be flat or turn sideways (cup-shaped nails). When cutting nails, it is good to be extra careful in this case.
Failure
Some girls with Turner syndrome have feeding problems in the first year of life - they suck less (the cause may be a more arched floor), chew and swallow, sometimes they may be more prone to vomiting or blinking than other children. Due to frequent vomiting, they may then gain poor weight. These problems usually go away before the end of the first year and do not cause any problems in the next life.
4. Turner syndrome in childhood
Grow
Not all of the above-mentioned manifestations of Turner syndrome are present in many girls - or they do not have to attract attention. Most girls with Turner syndrome benefit as well as other children and do not have noticeable health problems. Therefore, Turner syndrome often occurs later in childhood. The most common reason for finding Turner syndrome at this age is growth failure.
All girls with Turner syndrome grow more slowly than other children. The delay in growth is often noticeable in the first years of life, but it becomes more and more significant as the years go by. Already when they start school, girls with Turner syndrome are on average 17 cm smaller than other girls of the same age. Young women with Turner syndrome grow to an average height of 146 cm when left untreated. This is exactly 20 cm less than the average adult height of Czech young women. If a girl with Turner syndrome has tall parents, she can grow to a height of 158 cm and will therefore not differ in size from small girls without Turner syndrome. However, if she did not have Turner syndrome, such a girl would grow to a height of 178 cm. Conversely, the daughter of a young parent who has Turner syndrome can reach only 134 cm in some adult cases (instead of 154 cm if she does not have Turner syndrome).
Adult height of untreated women with Turner syndrome
ranges from 134 to 158 cm (diameter: 146 cm)
We still do not understand the reason for the small stature of girls with Turner syndrome. We know that these girls produce normal amounts of growth hormone in their bodies, but their growth hormone is not enough to ensure normal growth. The long bones of the limbs, which make a decisive contribution to growth throughout childhood, are less sensitive to growth hormone in girls with Turner syndrome.
For many years, therefore, it was thought that low height was the inevitable fate of every girl and woman with Turner syndrome and that she could not be affected by treatment. It was not until the late XNUMXs that the first promising reports emerged, suggesting that high-dose therapeutic administration of growth hormone could at least partially overcome the low susceptibility of long bones to growth hormone. Thus, another growth hormone began to be added to the growth hormone itself as a drug.
We now know that growth hormone therapy really helps girls with Turner syndrome. Although it cannot completely eliminate the growth disorder, it can significantly alleviate it and allow the vast majority of girls to reach socially acceptable body height on the threshold of adulthood. Since 1991, when growth hormone therapy was started in girls with Turner syndrome in the Czech Republic, it has been given to over 170 girls. Each year of treatment will help a little, but only long-term, long-lasting treatment brings the greatest benefit.
| diameter | range | |
|---|---|---|
| without growth hormone treatment | 146 cm | 134 - 158 cm |
| if the treatment lasted 1 year | 149,8 cm | 137,8 - 161,8 cm |
| if the treatment lasted 2 years | 151,9 cm | 139,9 - 163,9 cm |
| if the treatment lasted 3 years | 153,2 cm | 141,2 - 165,2 cm |
With each passing year of treatment, adult height continues to improve somewhat.
Growth hormone treatment is quite demanding. It is performed at selected pediatric clinics that have sufficient experience with this treatment. There are twelve such places in the Czech Republic. You can ask your pediatrician to see a specialist in growth hormone treatment.
Growth hormone is given by injection. It is a substance of a proteinaceous nature which, when administered in tablets, drops or syrup, would be disturbed by the digestive juices in the digestive tract and only its ineffective residues would pass into the blood. Therefore, the digestive system must be bypassed during treatment.
Growth hormone injections are given subcutaneously. This easiest way to give injections is easy for anyone to learn. Parents and older girls themselves will soon gain such skill in injecting that stinging is no bigger problem for them than brushing their teeth. In order for the body to benefit most from growth hormone, it needs to be given every day. The best time to inject is at bedtime. The reason is the fact that in every child, the growth hormone in the body is most produced in the first hours of the night after falling asleep, and the natural rhythm of the action of the growth hormone is faithfully imitated by injection before going to bed. In addition, we have enough peace to inject the night before bed, and if it becomes part of our daily evening activities, we will not forget it.
Growth hormone injections are almost painless. Special pens with a very thin needle are available for administration, which everyone can easily learn to operate.
Growth hormone therapy is always voluntary in girls with Turner syndrome. The decision to start treatment is the joint conclusion of the parents and the doctor. Parents should always be well informed before making their decision. They should understand the patterns of growth in girls with Turner syndrome and know that if the growth disorder is not yet noticeable in preschool age, it may be much more noticeable later, eg at the age of twelve - but delaying treatment has uncomfortably shortened the time the girl will grow and the overall effect of the treatment will no longer be ideal. The doctor should always acquaint the parents with the predictions of the adult height of their daughter. Such a prediction is not entirely accurate, but it will help for orientation.
We know from experience that most parents choose growth hormone therapy. Sometimes the purpose of treatment is considered by tall parents, whose daughter with Turner syndrome has a chance to grow up to a height of 158 cm without treatment. Parents may consider this adult height to be sufficient. However, even such a girl will grow more in the case of growth hormone treatment.
Many parents of girls with Turner syndrome ask about possible side effects before starting growth hormone treatment. Growth hormone is a substance in the body. As a drug, it is produced in a way that ensures that the final product is completely identical to its own growth hormone. From this point of view, treatment is safe.
The fact that we give more growth hormone than usual for the human body can be a problem. Indeed, increased amounts of growth hormone can have some side effects. However, from the experience of more than 170 girls treated to date in the Czech Republic, we can state that these side effects are not dangerous - and so far have not led to the need to interrupt treatment.
One of the possible side effects of growth hormone treatment is the retention of more water in the body. This usually does not lead to difficulties. However, if the girl had swelling of the insteps or hands (lymphedema) after birth, a sign of swelling may reappear after starting treatment. However, they only rarely cause greater problems.
It is also necessary to monitor the maintenance of blood sugar (glycemia) during growth hormone therapy. Your doctor will take responsibility for regular check-ups in this area (examination of so-called glycosylated hemoglobin, HbA1c). Girls with Turner syndrome are born with a slightly increased tendency to develop diabetes, and in some, mild diabetes actually manifests itself in adulthood. Growth hormone is known to increase the tendency to develop diabetes in some cases. Initially, therefore, we closely monitored all girls with Turner syndrome during growth hormone treatment. However, the experience is encouraging. An increased incidence of diabetes during growth hormone treatment has not been observed in our country or in other countries.
According to previous experience, growth hormone treatment in girls with Turner syndrome is therefore not only effective but also safe.
Hearing
Some girls with Turner syndrome may have noticeably frequent otitis media. The cause is a slightly deviating curvature of the Eustachian tube, which creates a connection between the middle ear cavity and the nasopharynx. In girls with Turner syndrome, even with small inflammation of the nasopharynx, the Eustachian tube may become temporarily blocked. An impenetrable Eustachian tube causes the feeling of a "lying ear" and impairs hearing. At that time, otitis media often begins to develop, which can lead to perforation (rupture) of the eardrum.
Often recurrent or lingering otitis media can cause long-term or even permanent hearing loss. Therefore, especially for girls with Turner syndrome, it is very necessary that their otitis media be recognized in time and treated thoroughly. Although we usually do not advise using antibiotics too often, it is always better to use antibiotics in order to manage the inflammation as soon as possible and to reduce the risk of its transition to a prolonged stage.
A little girl with Turner syndrome who has problems with otitis media should be monitored by a specialist ear doctor (otorhinolaryngologist) who has sufficient experience with similar children. Hearing impairment is not inevitable and can often be prevented by proper treatment.
Exceptionally, hearing loss in a girl with Turner syndrome may be congenital. That is why it is beneficial if the examination for Turner syndrome also includes an audiogram - an examination in which even a slight hearing loss can be recognized, even at certain pitches. Unrecognized and untreated hearing loss brings problems in speech development, later it can be one of the causes of school failures. At the same time, it is easy to face.
Air
Myopia or squinting occur in many children. They are only slightly more common in Turner syndrome, but they are treated similarly to other girls. If we recognize them in time, we will prevent further problems. Therefore, every family of a girl with Turner syndrome should have the opportunity to visit a specialized pediatric ophthalmologist (ophthalmologist).
Exceptionally, a decrease in the upper eyelids (ptosis) may also occur. It can impair visual well-being, forcing the head to tilt. Eyelid ptosis can be treated with plastic treatment.
Skin
Some girls with Turner syndrome have prominent pigmented spots (nevi) on their skin. Their number may increase slightly during growth hormone treatment. The development of large nevi should be monitored by a specialist in skin diseases - a pediatric dermatologist.
5. Girl with Turner syndrome at school
What are the mental abilities of girls with Turner syndrome?
By comparing the mental abilities of girls with Turner syndrome with their sisters, they were found to be completely intellectually comparable. This refuted a long-held prejudice about reduced mental abilities in Turner syndrome.
Girls with Turner syndrome perform better in intelligence tests in the verbal (verbal) component than in non-verbal (written, cartoon or mathematical) tasks. Their weaker side may be the lack of concentration and a somewhat worse spatial imagination, which is needed in solving mathematical problems.
How are they doing at school?
Most girls with Turner syndrome are successful at school. As with other children, the pupils are above average, average and below average.
However, for many of them, some features are common: They often learn to read earlier than other children, but the age at which they begin to write is a little later. Solving problems associated with spatial imagination, especially mathematical and geometric, can be a certain weakness. Teachers should be informed. However, they should not underestimate the girl and consciously place less demands on him than on others.
What are their relationships with classmates?
Due to their supportive nature, girls with Turner syndrome tend to have many friends at school and beyond, and are often very popular with classmates.
Are some character traits typical for them?
Typical character traits of girls with Turner syndrome include openness, diligence and zeal, conscientiousness, non-moodiness. Girls with Turner syndrome have a sense of order and take great care of their appearance, which is reflected in care in dressing, styling or facial hair.
A certain immaturity in the emotional area can accompany a girl with Turner syndrome through childhood and adolescence. She becomes an "adult" a little later than her classmates. Sometimes also because her family and surroundings consider her younger than she really is (mainly because of her smaller figure) and they try to "protect" her for longer. This approach does not contribute to the development of self-confidence, slows down emotional maturation, increases the girl's dependence on the family and thus, especially in adolescence, isolates her somewhat from her peers and assigns her to younger children. It will help a girl with Turner syndrome if her family, teachers and friends treat her appropriately at the level of her age and not her height. This also applies to dressing, involvement in extracurricular activities, requiring a certain degree of responsibility for the tasks performed and the like.
Recently, thanks to growth hormone treatment, which improves the height of girls, we encounter these problems less. They are mainly those in girls who have been diagnosed with Turner's syndrome late or who have not been started on growth hormone therapy.
Katka's mother, who has been going to our surgery since she was 9 years old, says: "Katka always had a lot of friends, but especially among younger children. I was happy because I thought she was happier among them. Interestingly, she always had a leading role in the group and was able to take good care of younger children, even though she looked just as old. When Katka went to the first grade and the pediatrician recommended postponing school attendance, we consulted a child psychologist, who disagreed. She started isolating herself from her classmates, and she missed a lot because she had recurrent otitis media, and she even had to be admitted to the hospital, where the doctor told me that she suspected our daughter had a genetic disorder. That it was not a disease, but rather a set of symptoms caused by the absence of a single chromosome. will continue. We kept asking new and new questions. The doctor talked to us repeatedly and for a long time - about further examinations, treatment, adolescence, adulthood. Very soon, Katka began treatment with growth hormone. During the first year of treatment, it grew almost 8 centimeters. Suddenly, we all watched in surprise as she became confident, joined her classmates, and even joined the Scout Squad. She is now almost 14 years old, one of the better students at the school and she would like to study at a medical school where she will not need so much math. He leads a scout unit, has a lot of friends and is no longer the smallest in the class ... "
Katka's mother told this story not only for herself, but for many other parents of girls with Turner syndrome.
6. Turner syndrome in adolescence
Adolescence (puberty) is the period when a child is born into an adult.
At the beginning of adolescence, the gonads (ovaries in girls) begin to produce sex hormones (estrogens in girls, later progesterone). Puberty begins with individual girls of different ages, usually between the ages of 9 and 13. The production of female sex hormones is initially small, but continues to increase during adolescence. Due to sex hormones, girls typically experience changes in their body shape. Growth accelerates, the mammary glands develop, the uterus and vagina enlarge, the pelvis widens, and adipose tissue begins to accumulate in typical landscapes of the body. At the peak of adolescence, the first months appear, which signals the beginning of regular (cyclical) production of hormones, which leads to the separation of the uterine mucosa at an interval of approximately 28 days, accompanied by bleeding (menstruation), lasting 3-5 days. All of these changes begin gradually, usually over 2-4 years.
The ovaries are therefore needed for development during adolescence. They produce female sex hormones and contain the base of eggs needed for future pregnancies. Little girls with Turner syndrome have normal-looking ovaries in the first months of their intrauterine life. Gradually, however, they begin to change and in most cases, they are unable to produce hormones or contain eggs. Therefore, the usual changes do not occur at the time of the expected onset of puberty. An exception is a small number of girls, who usually have a chromosomal mosaic in the karyotype. Their ovaries may work for a period of time, they may develop normal adolescence and may even have regular periods, and in rare cases may become pregnant.
With the exception of the ovaries, the internal and external genitalia of girls with Turner syndrome are completely normal.
Missing ovarian hormones can be replaced with appropriate drugs. Thanks to this, it is possible to induce puberty perfectly and maintain female maturity, including a regular menstrual cycle. This task is usually performed by a pediatric endocrinologist, later treated by a gynecologist.
When is the best time to start growing up?
During adolescence, a person is much more sensitive to his surroundings. The girls just want to be as well informed as possible about how their hormonal treatment will take place and what they can expect in the near future.
As we already know, individual girls without Turner syndrome begin to grow at different ages. Therefore, even for a girl with Turner syndrome, it is necessary to carefully choose the time when the induction of adolescence will be most appropriate. It is necessary to assess a number of circumstances and discuss them in detail with the girl and her parents, so that we do not rush the beginning of adolescence unnecessarily or delay it inappropriately. Estrogens given prematurely are known to shorten overall growth time and thereby reduce adult height. They lead to the closure of growth cracks in the long bones. Therefore, we recommend starting the administration of female hormones a little later. The appropriate time is not the same for all girls and can be determined from an X-ray of the wrist. Your doctor will tell you when it will be appropriate to start estrogen treatment so that the adult height suffers as little as possible. While we start growth hormone treatment as soon as possible, we usually postpone estrogen administration between the ages of 13 and 15. The reward is a gain of a few extra centimeters in height, at the cost of a slightly later shaping of the figure in a female direction. If a girl and her parents decide to grow up earlier, their views will be respected. Usually, however, girls with Turner syndrome do not rush into adolescence because they know classmates who also start growing up later.
We'll talk about treatment female sex hormones, but in reality it is not a cure, but a substitute for substances that the body cannot produce. The doses of female sex hormones are therefore very low at the beginning and are gradually increased very slowly (over 2-3 years) in order to mimic their natural production in other girls.
We start with the administration of estrogens alone. Gradually, breasts will begin to develop, subcutaneous fat will accumulate in typically female areas (buttocks and thighs), and sometimes a whitish discharge will appear, which may be a harbinger of the approaching first period. When the first bleeding occurs, your doctor should be informed immediately, as this is the time when hormonal treatment needs to be adjusted. To maintain a regular menstrual cycle, it is then necessary to combine the female hormones estrogen (given in the first half of the cycle) with another female hormone called progesterone (given in the second half of the cycle). As soon as a dose of hormones is found that suits the girl and during which she has regular and heavy menstruation, this treatment is left for a long time. It used to be recommended to take hormone replacement therapy until you were about 50 years old, but now we know that small doses of female sex hormones are beneficial even longer. Estrogens also have a protective effect on the heart and blood vessels and improve the storage of calcium in the bones. Therefore, their use is also recommended for other adult women after menstruation (after menopause). There are several products containing female sex hormones and they exist in various forms. The most common are pills, but it is also possible to use patches from which the hormone is absorbed through the skin. Each form has its advantages and disadvantages. All are usually well tolerated and have no major side effects. They are very similar to hormonal contraceptives used by millions of women around the world. Exceptionally, headache, stomach pain, water retention or chest tightness may occur when administered. The gynecologist will recommend the appropriate combination, whether it is the type of product, the dose and the time of administration, and can change it at any time according to individual tolerance. Treatment must be continuous, uninterrupted to achieve balanced hormonal levels, regular menstrual cycles and proper uterine size. The administration of female sex hormones also leads to the production of vaginal mucus and thus enables a completely natural sex life.
Every girl should keep her menstrual calendar. It records the period of menstruation, its abundance and possible difficulties - abdominal pain, headache, discharge and the like. The menstrual calendar can be obtained free of charge at any gynecologist's office, sometimes a pediatrician, endocrinologist or pharmacy. It belongs in the purse of every modern girl and woman.
Young girls often ask if regular gynecological examinations are necessary during treatment with female sex hormones. We usually recommend them about 1-2 years after starting the combination treatment, especially to make sure that the development of the genitals corresponds to age - previously only in case of severe problems. The good effectiveness of hormonal treatment can be assessed primarily by the degree of development in the female direction, by regular menstruation and by monitoring the levels of hormones in the blood. Sometimes it is useful to perform a painless ultrasound examination.
If the ovaries do not fulfill their function, is it not better to remove them?
Surgical removal of the ovaries is only recommended for girls who have a Y chromosome or part of it in their karyotype. In their exceptional case, they could start developing in the ovaries in an undesirable, detrimental direction. The most reliable methods of examining a blood cork test, which are becoming available in the departments of medical genetics, are used to determine whether a girl has this karyotype. The examination can be arranged by your doctor.
If a small fraction of the Y chromosome is detected, we recommend removing the ovaries. This is a simple operation, but it should not be postponed. There is no risk after the operation. Hormonal treatment is then conducted as in other girls, and the development is clearly moving in a female direction.
A common concern of parents, and at a later age of the girls themselves, is whether they are women in the true sense of the word, even if they lack one or part of their sex chromosomes. It is appropriate to reassure them that their feelings, temperament and behavior are purely feminine. Their relationship with the opposite sex is reasonable, only sometimes it can be affected by a certain emotional immaturity, which can be reflected in the establishment of partnerships and the later beginning of sexual life. It is usually full-value and is contributed to by normal levels of female sex hormones in the blood, whether produced naturally or supplied in the form of drugs.
7. Turner syndrome in adulthood
Parents help to solve most problems in childhood or adolescence. As an adult, a woman with Turner syndrome becomes independent and finds a partner. Some new problems are emerging, typical of adulthood. The care of paediatricians is ending and the young woman should find a specialist with their help who knows the issue of Turner syndrome well and will therefore not underestimate some problems or overestimate others unnecessarily. It will work with doctors in other fields, as it will be necessary to continue treatment initiated in childhood and adolescence, to monitor any previous associated medical abnormalities (such as hearing, vision, kidney and heart disorders), but also to face the difficulties that age can bring. adulthood. It is important that the care of a girl or woman with Turner syndrome is not interrupted, so that the woman is not left without "her doctor", whom she trusts.
Can a woman with Turner syndrome get pregnant?
We already know that the vast majority of girls and women with Turner syndrome do not have well-functioning ovaries. The role of the ovaries is both to produce female sex hormones and to release eggs into the fallopian tubes, which are ready for fertilization by the male germ cell - sperm. Therefore, most women with Turner syndrome cannot get pregnant naturally. Rare exceptions are women with chromosomal mosaics and most cells with karyotype 46, XX. However, even their possible pregnancy carries with it the risk of birth defects or chromosome disorders in the fetus, so it must be monitored both by a gynecologist and at a specialized workplace of medical genetics.
And what about other women who have a partner and long for a child?
There has been a possibility for several years artificial insemination (in vitro fertilization - IVF) sperm eggs outside the mother's body. This is how "children from the test tube" are created, of which thousands have already been born in the world. This procedure is often used in cases where a woman forms eggs but they cannot be fertilized in a natural way. The egg is taken with a special device and fertilized with the sperm of the woman's partner. At other times, this procedure can be used for male infertility - the collected egg is fertilized in the test tube with the donor's sperm. In all cases, the fertilized egg returns to the mother's uterus, and if it nests there successfully, the woman experiences a natural pregnancy.
At present, our laws allow not only the donation of male germ cells (sperm), but also the donation of eggs. The egg donor is an anonymous healthy woman who has no hereditary burden in the family. She undergoes an examination in a genetic clinic and is also examined for karyotype.
Such donated eggs can also be used for artificial insemination of a woman with Turner syndrome. They can also be fertilized in the test tube with the sperm of their own husband. The condition for successful nesting of a donated egg in the uterus of a woman with Turner syndrome is an adequate size of her uterus. Prior long-term and regular administration of female sex hormones is therefore essential. Pregnancy must be maintained by supplying hormones until their own placenta takes over. Throughout such a pregnancy, the woman is regularly checked - in addition to routine examinations, blood hormone levels, blood sugar levels (blood sugar), urine and blood pressure are monitored. The size of the fetus, its growth and development are checked by ultrasound.
Recently, the transfer of a donated egg has been preferred to spontaneous pregnancies even in those women with Turner syndrome who exceptionally make eggs. The reason is a lower probability of congenital malformation of the fetus. Each gynecological, genetic or endocrinological center will provide information on specialized centers for this type of artificial insemination. The success rate of egg transfer is currently between 25 and 30%.
For some women, artificial insemination is not suitable for health reasons, others reject it, for example for religious reasons, and for some they fail even after repeated attempts. The solution can then be one of the types adoption child (adoption or foster care). Information on adoption options will be provided by the attending physician or the substitute family care department at the city or district office. Both in artificial insemination and in the adoption of a child, a woman needs to be married or have a partner.
Osteoporosis
Osteoporosis can be one of the problems of women with Turner syndrome. By this we mean a gradual loss of calcium in the bones and a reduction in their strength. This problem affects most women in old age, but with Turner syndrome tends to come earlier. It was originally thought that the cause was the lack of female sex hormones. Today we already know that a different bone structure is also involved. Osteoporosis can cause unpleasant problems - pain or even more frequent fractures in minor injuries or sports.
How can osteoporosis be detected?
In recent years, there has been a very accurate and non-burdensome examination of bone mass. It's called densitometry, or measuring bone density. It resembles an X-ray, but does not expose a person to a significant dose of radiation. As a rule, the most congested areas of the skeleton, especially the lumbar spine, are examined.
Can osteoporosis be treated?
Growth hormone therapy alone in childhood has a positive effect on bone condition. It also helps to administer female sex hormones. Lifestyle also plays an important role. The diet should be rich in calcium, which is mainly found in dairy products. It can also be used in the form of tablets, sometimes a small dose of vitamin D is added to it. Regular recreational sports are very suitable for the prevention of osteoporosis.
Other health problems
It is more common in women with Turner syndrome higher blood pressure (hypertension). The cause can be both an unrecognized heart defect and congenital kidney defects or abnormal vascular formation. In some women, the cause of the higher blood pressure is not identified.
Tendency to higher blood sugar levels (higher glycaemia) is slightly more common in women with Turner syndrome than in other women. However, typical diabetes rarely develops. As a precaution, girls and women with Turner syndrome are advised not to overeat sweet and maintain optimal body weight. The slim figure in combination with appropriately chosen clothing and extra accessories seemingly adds a few extra centimeters to each woman.
It may be more common in women with Turner syndrome decreased thyroid function. This disorder does not hurt, but it can make life miserable because it reduces physical and mental performance. Healing is relatively easy. Therefore, it pays to check thyroid function once a year by blood sampling.
With increasing age, the tendency to wound heals increases stiffer (keloid) scars. This should be kept in mind by women who opt for plastic surgery, for example - drooping eyelids, skin lashes on the neck, pigmented nevi.
8. Is Turner syndrome a disease?
We don't consider Turner syndrome to be a disease. Rather, it is a set of symptoms and difficulties that are not permanent and can usually be successfully addressed. Congenital malformations (kidneys, heart, neck lashes and others) can be operated on and will no longer manifest for the rest of your life. Today, we also treat growth retardation and ovarian dysfunction, mostly with good results. The current young generation of girls and women with Turner syndrome will no longer face the problems that have plagued women in the past, when treatment options were still limited.
It is important to recognize Turner syndrome as soon as possible. It can not only be treated in time and therefore more successfully, but also soon and truthfully inform the parents and later the girl about the cause of her difficulties. It is the duty of the physician to provide comprehensive information and the duty of the parents or later of the girl or woman herself is to request further information. But not everyone finds the courage to ask openly during their first contacts. Some questions may seem unnecessary at first, others are embarrassing. This text should therefore also provide little help.
I AM ME
(Title track of Lenka Kosinová's CD of the same name - the first CD sung by a woman with Turner syndrome. The text was written by Ilona Rybářová.)
If I were the wind from the mountains,
what the dust tolerates in the valley,
the wind what he says
I would not be afraid from afar.
If only I could for a while
see the trees bloom in the sun
perceive the rainbow of butterflies,
I would be punished for that.
But I'm me,
so let me be no more
I have to give you strength
your love, otherwise nothing.
If I were a meadow in bloom,
where children go to play,
she whispered her songs to them,
she learned to know them.
If I were a river of stones,
the river that found the dam,
its power from the springs
I would spill you.
I'm me,
so let me be no more
I have to give you strength
your love
and with her I go to meet you.
Some prejudices that a girl or woman with Turner syndrome may encounter
Prejudice: Girls with Turner syndrome have a reduced intellect.
Explanation: It's not true. When comparing the intellectual abilities of girls with Turner syndrome and their sisters without Turner syndrome, they were found to have comparable intellect. Some girls with Turner syndrome may have certain mathematical difficulties due to their less spatial imagination. In other areas, however, other girls outperform, as we discuss in the relevant chapter.
Prejudice: Growth hormone therapy does not make sense because low altitude in Turner syndrome cannot be affected.
Explanation: It's not true. Reports of growth hormone therapy have been reported in the early XNUMXs, when completely inadequate doses were given. Currently, the beneficial effect of growth hormone treatment on adult height is clearly demonstrated.
Prejudice: A girl with Turner syndrome can't play sports.
Explanation: It's not true. Girls with Turner syndrome can be as successful in many sports as their classmates. The handicap can only be a smaller height, so it is appropriate to choose the sport judiciously.
Prejudice: Women with Turner syndrome do not have a natural sexual feeling.
Explanation: It's not true. Women with Turner syndrome have the prerequisites for establishing natural partnerships just like other women. They do not have increased homosexuality or other abnormalities. Sexual sensation in them is enhanced by the administration of female sex hormones, which is a natural part of ovarian function replacement.
Prejudice: A woman with Turner syndrome can never give birth.
Explanation: It's not true. The uterus develops in women with Turner syndrome in the same way as in other women, and thanks to the administration of female sex hormones, it also reaches its usual adult size. After transferring a fertilized egg to the uterus (artificial insemination, in vitro fertilization), a woman with Turner syndrome can experience pregnancy and give birth.
Usual medical monitoring and treatment of girls and women with Turner syndrome
When detecting Turner syndrome:
- ultrasound examination of the heart and large vessels (echocardiography)
- ultrasound examination of the kidneys and urinary tract
- ear and eye examinations
- examination of thyroid function (blood sampling)
- growth and adult height prediction
- joint decision of the doctor and parents on growth hormone treatment
During growth hormone therapy:
- growth rate controls
- regular thyroid function tests (blood sampling)
- elimination of diabetes (blood sampling)
Before the usual age for adolescence:
- determination of ovarian function (blood collection)
- determination of bone maturity (X-ray of the wrist)
- decision on treatment with female sex hormones (gynecological examination is not necessary)
In adulthood:
- usually permanent treatment with female sex hormones (in the care of a gynecologist)
- regular thyroid function tests (blood sampling)
- elimination of diabetes (blood sampling)
- blood pressure monitoring
- monitoring of bone strength
More detailed examination may be needed for girls who have been found to have deviating findings or who have other health problems.
Glossary of technical terms
amniocentesis - amniotic fluid collection during pregnancy for genetic testing
autosomes - chromosomes that look the same in women and men
cubiti valgus - limited ability to stretch the arms at the elbows in a straight line
densitometry - bone density measurement
echocardiography - ultrasound examination of the shape and structure of the heart
estrogens - An important group of female sex hormones that are produced in the ovaries
Jan - the chemical structure in which the hereditary (genetic) information is recorded
heterochromosomes (gonosomes, sex chromosomes) - chromosomes that determine a person's gender. A pair of sex chromosomes XX is typical for women and XY for men. Girls with Turner syndrome often have only one X chromosome
hormone - chemical messenger inside the human body. It transmits information from the place of its origin to the so-called target tissues, the activity of which it regulates
chromosome - a unit in the cell nucleus that contains genes
chromosomal mosaic - a mixture of two or more different sets of chromosomes in cells of the same human
in vitro fertilization (IVF) - artificial insemination of an egg with sperm outside the mother's body. The egg is then fed back into the mother's uterus
karyotype - a set of chromosomes in the nucleus of every cell in the human body. Karyotype testing is necessary to diagnose Turner syndrome
aortic coarctation (narrowing of the heart) - congenital abnormality, which may occur in some girls with Turner syndrome. Narrowing is a barrier to blood flow to the lower half of the body, and the heart must work hard against high resistance. Aortic coarctation can be operated on
cordocentesis - collection of fetal umbilical cord blood during pregnancy for genetic testing
lymphedema - swelling in case of insufficient outflow of tissue fluid (sap, lymph). In Turner syndrome, lymphedema can affect the backs of the hands and insteps. They are usually transient and disappear during the first year of life
osteoporosis - loss of calcium in the bones and reduction of their strength
placenta - fruitcake. The organ inside the uterus through which the fetus receives oxygen and nutrients from the mother's body. Also the place of origin of hormones important for the course of pregnancy
horseshoe kidney (ren arcuatus) - congenital kidney disease, which occurs in some girls with Turner syndrome. He only rarely causes difficulties
progesterone - one of the female sex hormones
pterygium colli - skin fold (doubling of the skin) laterally on the neck. May give the impression of a wide neck.
ptosis - drop of upper eyelids
puberty - adolescence. The birth of a child into an adult
sperm - mature male germ cell
syndrome - set of flags
structural anomalies - deviating shape
ultrasound (sonography, ultrasonography) - examination method in which the internal organs of the human body are imaged on the principle of ultrasonic waves. Completely painless and harmless examination
egg - mature female germ cell
Specialist doctors a girl and a woman with Turner syndrome may encounter
allergist - specialist in the treatment of hypersensitivity diseases
endocrinologist - specialist in the treatment of hormonal disorders. He usually coordinates the care of a girl and a woman with Turner syndrome
dermatologist - specialist in the treatment of skin diseases
gastroenterologist - specialist for the treatment of diseases of the digestive system
genetic - specialist for the detection of hereditary and congenital diseases. Significantly involved in the diagnosis of Turner syndrome
gynecologist - specialist for the treatment of diseases of the female genital organs
cardiologist - specialist in the treatment of cardiovascular diseases
nephrologist - kidney disease specialist
ophthalmologist - specialist in the treatment of eye disorders
otolaryngologist - specialist for the treatment of diseases and disorders of the ears, nose and larynx
urologist - specialist in the treatment of urinary tract diseases
History of Turner syndrome in data
1768
Dr. Giovanni Battista Morgagni, considered the father of the scientific conception of medicine, described in a deceased woman in whom he performed an autopsy, symptoms resembling Turner syndrome - small stature, deviating kidney formation and lack of ovarian tissue. His findings have been overlooked by the medical community for more than 150 years.
1883
Dr. Kobylinski described a male patient with lashes on his neck. For many decades, this has called into question the true nature of Turner syndrome, which only affects women.
1902
Dr. Funke published the observations of a 15-year-old girl with a small figure, lack of adolescence, skin lashes on the neck, swelling of the legs, but also other manifestations of Turner syndrome - low-set ear lobes and a high, arched palate.
1929
Dr. O. Ullrich reported at the Munich Society of Pediatrics about an eight-year-old girl with symptoms of Turner syndrome. Therefore, in Germany, Turner syndrome is still called Ullrich-Turner syndrome.
1938
Dr. Herny Turner, an internist in Oklahoma City, wrote an article in a reputable trade magazine describing more girls and women with symptoms of Turner syndrome. He has been bearing his name ever since. Later, Dr. Turner pioneered the administration of female sex hormones to these women. For the first time, they could be helped effectively.
1959
Dr. Ford has developed a method for examining karyotypes and has shown that the absence of X chromosome is the cause of Turner syndrome.
1970
Dr. Turner died at the age of 78.
1981
The first Turner Syndrome Society was formed in Toronto, Canada. Its aim was to spread knowledge about Turner syndrome among the families of affected girls, among adult women with Turner syndrome, but also among the medical community. Today, Turner Syndrome companies or clubs exist in many dozens of countries around the world, providing empowerment and assistance to thousands of Turner Syndrome carriers.
1985
The first woman with Turner syndrome became pregnant thanks to a donated egg.
1986
Research into the effectiveness of growth hormone therapy in Turner syndrome has begun in the United States and Europe.
1989
The Club of Girls and Women with Turner Syndrome was founded in Prague. Its members are girls and women from all over the Czech Republic. Club address: 160 00 Prague 6, Kladenská 1.
1990
The club started publishing the magazine "Téčko".
1991
Launch of the first Czech study with growth hormone in ten girls with Turner syndrome.
1992
Growth hormone treatment has become available to girls with Turner syndrome throughout the Czech Republic.
1996
Lenka Kosinová's CD "I am me" is released - the first CD sung by a woman with Turner syndrome.
1997
The first woman with Turner syndrome in the Czech Republic gave birth to a baby from a donated egg.
1998
Lenka Kosinová is preparing the release of the second CD entitled "Stay on top of things"
Authors
Prof. MD Jan Lebl, CSc. (born 1955) is the head of the Pediatric Clinic of the 2nd Medical Faculty of Charles University and the University Hospital in Prague-Motol. He graduated from the Medical Faculty of Charles University in 1980. He defended his dissertation on "Diagnosis of children with growth disorders" in 1990 and the habilitation thesis "Treatment with growth hormone" in 1993. He cares for children with growth and development disorders, diabetes and other endocrine diseases. In 1989, he initiated the establishment of the Club of Girls and Women with Turner Syndrome. In the early 1996s, together with other Czech and Moravian pediatric endocrinologists, he was responsible for the introduction of growth hormone therapy in these girls. He is the author of the monograph "The Growth of Children and Its Disorders" (1997), several books for parents ("The Growth and Maturation of Your Child" - XNUMX and others) and many articles in the professional press. It emphasizes the patient's active approach to his health problem. He is a supporter and promoter of the idea that parents and children should be well informed about their health, should understand it well, and should be able to choose a doctor who will provide them with care at the level of current medical science.
Contact adress: Department of Pediatrics, Charles University, 2nd Faculty of Medicine and University Hospital Motol, V Úvalu 84, 150 06
Prague 5Doc. MUDr. Jirina Zapletalova, Ph.D. (born 1954) is an associate professor at the Children's Clinic of the Medical Faculty of Palacký University in Olomouc. She graduated from the Medical Faculty in Olomouc in 1979. She has been involved in pediatric endocrinology for over twenty years, and has been specializing in the treatment of children with growth and adolescence since the mid-2003s. She is one of the most active members of the Working Group for Growth Hormone of the Czech Endkorinological Society, is a member of a number of domestic and international medical societies (eg Growth Hormone Research Society) and represents the Czech Republic in the KIGS international growth study committee. She has lectured at home and abroad and published a number of articles in professional literature. She is the main author and organizer of the first Czech monograph on Turner syndrome, which was published in XNUMX.
Contact adress: Department of Pediatrics, University Hospital, IPPavlova 6, 775 20 Olomouc
For diabetics
Section 1
- What is diabetes? [doc; 41,5 kB]
- Talking about insulin [doc; 75,3 kB]
- Insulin program [doc; 47,6 kB]
- How we measure blood glucose at home [doc; 42,5 kB]
- Hypoglycemia [doc; 20,5 kB]
- We adjust the insulin dosage [doc; 46,1 kB]
- Ketones [doc; 55,8 kB]
- Vomiting [doc; 19,5 kB]
Section 2
- Our essential nutrients [doc; 20,5 kB]
- Exchangeable unit [doc; 35,3 kB]
- We know food [doc; 93,2 kB]
- Artificial sweeteners [doc; 31,2 kB]
Section 3
- Sport [doc; 55,8 kB]
- Smoking [doc; 13,8 kB]
- Alcohol and glycemia [doc; 45,1 kB]
- Investigation [doc; 37,4 kB]
- Late complications of diabetes [doc; 17,9 kB]
Section 4
- Diabetes of young children (guide for parents) [doc; 20,0 kB]
- Diabetes at school (teacher's guide) [doc; 15,4 kB]
- Adolescence and diabetes (guide for all involved) [doc; 20,5 kB]
- With diabetes on the go (travel guide) [doc; 53,8 kB]
- Will I have healthy children? (guide for future mothers) [doc; 31,2 kB]
- The future cure for diabetes (guide for curious and inquisitive) [doc; 28,7 kB]
- Four seasons with diabetes [doc; 38,4 kB]
Glossary
Glossary of technical terms [doc; 15,4 kB]
Authors of texts on childhood diabetes
- Prof. MD Jan Lebl, CSc. (born 1955)
Head of the Department of Pediatrics, 2nd Faculty of Medicine, Charles University and University Hospital in Prague-Motol - MUDr. Stepanka Pruhova, Ph.D. (born 1973)
researcher at the Department of Pediatrics, 2nd Faculty of Medicine, Charles University and University Hospital in Prague-Motol - Radka Šitová (born 1974)
educational and dietary nurse of the diabetology department of the Pediatric Clinic of the 2nd Faculty of Medicine, Charles University and the University Hospital in Prague-Motol - Helena Francová (born 1961)
educational nurse of the Department of Children and Adolescents of the 3rd Faculty of Medicine, Charles University and the Royal Vinohrady University Hospital - Jana Komárková (born 1965)
diet nurse of the Department of Children and Adolescents of the 3rd Faculty of Medicine, Charles University and the Royal Vinohrady University Hospital - Prim. MUDr. Jaroslav Skvor, CSc. (born 1955)
Head of the Children's Clinic of Masaryk Hospital in Ústí nad Labem
Premature adolescence
Download full text: Premature adolescence [doc; 603 kB]
Home
Premature adolescence is a general term encompassing not only premature puberty but also other disorders. We talk about it when the development of sexual characteristics begins in girls before the age of 8 (development of breasts, genitals or pubic hair = hair around the genitals) or axillary hair (underarms) and 9 years ago in boys (development of genitals, hair).
This text was created to help you understand both normal and premature adolescence and their variants. It will help you get acquainted with some medical terms, with treatment and with the possibility of family participation in the treatment.
Control of hormone production in the body
Hypothalamus is the part of the brain that is located above the pituitary gland, the hypothalamus is connected to the pituitary gland by a so-called stalk. With the help of regulatory hormones, the hypothalamus has a controlling - regulatory significance for the release of hormones of the anterior pituitary gland. The hypothalamus also produces a hormone that regulates water absorption in the kidneys and a hormone related to childbirth and lactation (to the production of breast milk).
Hypophysis or brainstem is a gland the size of a pea. This gland is often referred to as the "master gland." A number of hormones are formed in its anterior lobe, which are essential for the control of hormonal production in other endocrine glands. It is a growth hormone, hormones that control the function of the thyroid gland, adrenal glands or gonads. The posterior lobe of the pituitary gland serves as a reservoir for other hormones that are formed in the hypothalamus (a hormone that regulates water absorption and a hormone related to childbirth and lactation).
Hormones
They are chemicals released into the blood from the relevant endocrine glands. Their function is to transfer information between cells and maintain normal bodily functions. Many hormones are produced in the body: for example, the already mentioned thyroid hormones, growth hormone, sex hormones, adrenal hormones, insulin and others. The following hormones control adolescence (or puberty):
GnRH
gonadotropin releasing hormone (hormone releasing gonadotropins) is formed in the hypothalamus, controlling the production of hormones called gonadotropins. We also discuss gonadotropins elsewhere. Gonadotropin releasing hormone plays a key role in controlling puberty and fertility.
Gonadotropins
is formed in the cerebral cortex under the controlling influence of GnRH (gonadotropin releasing hormone). These are hormones called FSH and LH.
FSH: or follicle stimulating hormone supports the testes to produce male germ cells (sperm) and ovaries to develop female germ cells (eggs, oocytes) and together with luteinizing hormone supports the production of female sex hormones.
LH: luteinizing hormone supports the production of male sex hormones in the testes and, together with FSH, supports the production of female sex hormones in the ovaries.
Sex hormones
Testosterone in men and estrogens in women are responsible for the development of secondary or secondary sexual characteristics and for behavioral changes.
Testosterone: is a male sex hormone that is produced in the testicles of boys and adult men. Until puberty, his production is low. To a much lesser extent, it is also formed in the gonads of women, where it is a direct precursor and source for the production of female sex hormones.
However, other and much weaker male-acting hormones (androgens) are also produced in the human body in the adrenal glands, which are glands located in close proximity to the kidneys. These hormones affect not only the development of pubic hair (which means hair around the genitals), but also axillary hair (armpit hair) in both boys and girls.
Estrogens: are female sex hormones that affect the development of the breasts and uterus in girls, the place of production is the ovaries. Some androgens are a precursor to the normal production of estrogens in the ovaries. In hormonal disorders of adolescent girls and adult women, their excess may manifest certain symptoms, including menstrual disorders. Lower estrogen levels are also produced in boys by conversion from male sex hormones. In some boys, breast enlargement occurs during adolescence, which usually resolves spontaneously.
Normal puberty (normal adolescence)
Levels of gonadotropins (FSH and LH) and sex hormones are known to be high not only in adolescents but also in normal healthy newborns. This period is also called "mini-puberty". A significant decrease in hormonal levels occurs after 3-6. months. Testosterone levels in boys can be up to half in "mini-puberty" compared to adult men. In the period between 4 and 6 years of age, the production of gonadotropins and sex hormones is very low, with a slight increase occurring in 7-8 years.
Hormonal changes in puberty take place gradually, the development of secondary sexual characteristics begins after reaching the threshold values of hormonal levels. The rise in sex hormone levels begins several years before the development of secondary sexual characteristics.
Puberty is a change in the maturation of the gonads, that is, the testicles in boys and the ovaries in girls. As already mentioned, until puberty, sex hormone levels in boys and girls are very low, their rise affects the development of secondary sexual characteristics and stimulates pubertal growth acceleration. Puberty ends with fertility (sperm production in boys and egg maturation in girls).
Under normal circumstances, puberty in girls begins between the ages of 10 and 13. The first visible manifestation is usually the beginning of the development of the mammary glands and thus the enlargement of the breast, followed by the development of pubic hair. However, it can also be the other way around (the development of pubic hair can precede the development of the mammary glands). The first menstrual bleeding in girls usually occurs between the ages of 11 and 14. The normal range is 10-15 years, most often the first menstrual bleeding (menarche) occurs in our girls aged 12,5-13 years.
In boys with normal sexual development, the testicles enlarge first, then the penis (genitals, genitals) and pubic hair appears. These changes occur between the ages of 10 and 14. Underarm hair, beard growth and deepening of the voice occur in boys typically between the ages of 13 and 16.
The average age of onset of puberty differs by only 6 months for girls and boys, but it can be a difference of several years. This difference may also be related to the well-known experience that early signs of puberty in boys tend to be less noticeable than in girls. Testicular enlargement usually escapes the attention of parents, breast augmentation in girls is obvious and is therefore not overlooked. Although the progression of adolescence is the same for children, the time required for complete maturation ranges from 18 months to 5 years.
Growth acceleration in puberty depends on the production of growth hormone and sex hormones. When one of these hormones fails, the growth spurt is disrupted. In girls, growth accelerates (growth rate - spurt) soon after adolescence, after menarche growth grows. In boys, growth spurt begins later, around mid-puberty.
IF PUBERT APPEARS TO GIRLS BEFORE 8 YEARS AND TO BOYS BEFORE 9 YEAR, IT IS NECESSARY TO SEARCH FOR A SPECIALIST AND TO DETERMINE THE CAUSE OF PRE-ADMINISTRATION. ATTENTION AND THE EXAMINATION DESERVES THE BEGINNING OF PUBERTY IN GIRLS BETWEEN 8.-9. YEAR AU BOY BETWEEN 9.-10. ROKEM.
Glands that control adolescence
Glands and hormones affecting puberty
True premature puberty
True precocious puberty may also be referred to as gonadotropin-dependent (ie, gonadotropin-dependent) central precocious puberty. In most cases, it is idiopathic central premature puberty, which means premature adolescence for an unknown cause.
As already mentioned, precocious puberty indicates the onset of adolescence earlier than usual. In true premature puberty, hormonal regulation and the pattern of sexual development coincide with normal puberty, in contrast to the condition referred to as pseudopuberty, which we will discuss elsewhere.
The difference between normal and central premature puberty lies only at the time of onset of puberty.
A premature adolescent may initially be taller and more powerful overall than his or her peers and classmates. Weight gain is associated with premature pubertal growth acceleration (growth spurt). Bone maturation is also accelerated, indicating the biological age of the child (determined from an X-ray of the left wrist and hand). The bone age of the child reflects the prospect of further growth, so we can approximately determine the child's height in adulthood - it is a determination of growth prognosis. Higher growth of a premature adolescent does not mean that this child will be tall in adulthood. Conversely, if treatment is not started in time, growth crevices may close prematurely, growth may stop prematurely, and they may grow smaller than inherited. The goal of treatment is therefore not only to stop premature pubertal development, but also to delay the closure of growth crevices and prolong growth time.
Let us now turn to the other problems that accompany early adolescence. These are changes in the psyche and behavior. These problems do not occur in other children until normal puberty. For example, premature interest in the opposite sex, excitement, self-repentance (masturbation). There are also problems with concentration disorders at school and with integration into the children's team.
In most children, the cause of central precocious puberty is unknown. Activation of the hypothalamic - pituitary - gonadal axis (gonads) and premature male or female sexual development occur earlier than usual. Rarely, cysts or tumors in the lower brain, other diseases of the brain and central nervous system may be the cause of premature adolescence, or they may be a secondary manifestation and consequence of another disease and its treatment. Therefore, in addition to specialist examinations, your pediatrician may also recommend X-rays of the head, CT (computed tomography) or MR (magnetic resonance imaging) to clarify the diagnosis. Brain cysts and tumors causing true premature puberty are more common in boys than in girls, so a detailed examination in boys is always essential. True premature puberty is about 10 times more common in girls than in boys, with late puberty the opposite is true.
Gonadotropin-independent premature puberty
(gonadotropin-independent premature puberty)
This is a premature development of sexual characteristics due to the production of sex hormones, but by a different mechanism than in normal puberty. The cause is a disease of the adrenal glands or gonads (cysts, tumors, a disorder of hormone production in a congenital enzyme disorder). Differentiation is usually possible due to a different order of development of secondary sexual characteristics than in normal puberty (for example, hair development in boys without testicular development). The treatment of these conditions is aimed primarily at eliminating the cause, and thus at eliminating the source of sex hormone production.
Gonadotropin-independent premature puberty occurs in both girls and boys. It may be part of McCune-Albright syndrome (where other endocrine disorders often occur, bone and skin changes may also be present). In a condition called testotoxicosis, the testes develop prematurely, but without concomitant pituitary stimulation, unlike true central premature puberty. This disorder is more common in some families. The treatment is fundamentally different from the treatment of true premature puberty, although the symptoms and course of premature adolescence in testotoxicosis are similar to those in true premature puberty. In boys, premature pseudopuberty may also be due to some hormonally active tumors of the brain, liver, testes and adrenal glands, or it may be a manifestation of increased androgen production in the adrenal glands due to a hormonal disorder. Girls with ovarian cysts, hormonally active adrenal and gonadal tumors may also have premature pseudopuberty, as in boys with hormonal disorders and increased androgen production in the adrenal glands.
Other variants of premature adolescence (incomplete forms)
Premature telarché:
is a trivial and time-bound process. This is a unilateral or bilateral premature breast development. It occurs most often in girls during infancy and can last up to 3-4 years. The onset may be in the first months of life due to maternal hormones that pass into the milk, in which case the telarche usually subsides after breastfeeding. Premature telarche can also occur due to the production of their own ovarian estrogens, either in normal healthy girls with a slower onset of hormonal regulation. Estrogen-producing ovarian cysts have been found in some girls. However, it can also be an increased sensitivity of the mammary glands and breast tissue to estrogens, the levels of which do not exceed normal levels in the body. The possible effect of dietary estrogens is sometimes considered (not clearly established).
At the same time, there are no other manifestations of premature adolescence, the girl's growth is normal.
Breast size may vary (enlarge and shrink) at 4-6 week intervals.
It is necessary to distinguish this insignificant diagnosis from true premature puberty. No treatment is required for premature telarche, only regular monitoring is performed. This condition usually "goes off" within one or two years. Growth and definitive height are not adversely affected. Puberty starts at normal age, fertility is normal. This condition is probably known to many parents because many mild cases do not seek professional examination.
Premature adrenarchy:
is a harmless and time-limited matter. This is the development of pubic hair and / or axillary hair (armpit hair), usually starting between 6-9 years of age, in both boys and girls. Pubic hair here precedes the development of other pubertal features, that is, the development of the penis and testicles in boys and the development of breasts in girls, which starts at the usual age.
There may be a slight acceleration of growth along with a slight and insignificant acceleration of bone age. This is a normal manifestation of adrenal development, the condition requires no treatment, only monitoring.
It is diagnostically important to distinguish this insignificant form of premature adolescence from true premature puberty or from premature pseudopuberty, which may be associated with adrenal cysts or tumors, as previously mentioned. Sometimes a more detailed endocrinological examination (outpatient or short hospital stay) is necessary to clarify the nature of this deviation.
Isolated premature menarche:
These are rare cases of girls who start menstruating before the age of 10 without further signs of sexual maturation. The bleeding can be one-time or repeated at regular intervals for several years and then disappears. At the usual age, normal puberty occurs, including the onset of menstruation. The diagnosis can be made by a specialist only after excluding other causes of premature production of female sex hormones and / or after excluding another cause of vaginal bleeding.
Treatment of premature puberty
A. GnRH analog
(gonadotropin releasing hormone analogues or gonadoliberin analogues) (Decapeptyl depot, Diphereline, Lucrin)
Drugs in this group are chemicals that have some of the natural structure of the gonadoliberin molecule (GnRH). They are designed to block the effect of the naturally occurring hypothalamic hormone gonadoliberin (GnRH). With the help of these drugs, the binding sites in the cerebral cortex (or pituitary gland) for gonadoliberin, which is formed in the body, are occupied. The pituitary gland therefore subsequently reduces the production of gonadotropins (FSH and LH), the stimulation of the gonads decreases until it stops, and the production of sex hormones reaches prepubertal levels. The decline and normalization of hormonal levels is manifested by blocking changes typical of central or true premature puberty. No side effects have been reported with these drugs. Treatment must be carried out without interruption, according to the instructions of a specialist. Discontinuation of treatment leads to support rather than cessation of adolescence. Shortly after starting treatment, before the onset of a beneficial effect of treatment, transient manifestations of mildly progressing puberty may be transient. These include acne, mood swings, a slight increase in breast size, short vaginal bleeding (separating uterine bleeding from a drop in hormonal levels) or rather so-called "spotting". These symptoms disappear within a few weeks of starting treatment. Gonadoliberin analogues are now given in depot (long-acting) intramuscular injections once every 1 days; in some patients, injectable forms that are given once every 28 months can be used. The relevant pediatrician, which is either a pediatric endocrinologist or a pediatric gynecologist, will select the most suitable preparation and method of treatment for your child. Normally, injections are given at 1-day intervals, but may be shorter at the start of treatment. The most suitable treatment cycle is determined for each child by an expert.
B. Cyproterone acetate (Androcur)
This drug acts mainly at the level of the gonads (ovaries and testes), where it prevents the production of male and female sex hormones. It is made as tablets and is usually given 2-3 times a day. In the recent past, its efficacy for the treatment of true (central) puberty has been shown to be insufficient, and thus less suitable than the gonadoliberin analogs mentioned above. Therefore, it has not been used for several years for the treatment of central precocious puberty. An exception may be short-term transient treatment to delay the onset of menarche for various reasons.
Cyproterone acetate is an important drug for another form of precocious puberty that is not dependent on gonadotropins. This drug successfully suppresses the development of premature adolescence, but does not sufficiently reduce the development of bone maturation and therefore does not improve definitive body height.
Cyproterone acetate also affects the production of the adrenal ('stress') hormone cortisol, so adrenal function must be monitored during long-term treatment with higher doses and in some cases cortisol injections must be given to support the body in severe illness or surgery.
C. Other treatment
In some children with a high probability of low adult height, concomitant treatment with a gonadoliberin analogue and growth hormone may be appropriate. These are mainly children with severe growth failure due to intrauterine growth retardation, or children with proven insufficient production of growth hormone. In such cases, delaying the onset of puberty is an advantage, it allows for a prolongation of the growth time (later growth of the growth plates occurs and thus the closure of the growth slits). Research in this area continues.
Social issues
Your child is now probably taller than his peers. It is therefore natural that the environment is considered older. Don't forget his real age and don't overload him with tasks that are excessive for him. Your friends and teachers must also take this into account.
Premature adolescence brings with it a number of social problems. For example, a two-year-old child with premature puberty may look like a five-year-old. However, he has typical behavior for his age, wears diapers, does not completely maintain cleanliness. Mental development corresponds to the actual age of the child, but he looks much older. Premature sexual activity can manifest itself, for example, in erections in boys, masturbating. This attracts the attention and embarrassment of adults. Sweating, acne, and a change in body odor can also manifest as premature adolescence. In that case, we recommend more frequent bathing and washing of hair, skin care.
Children want to look and behave like their peers, and manifestations of premature adolescence often cause confusion and feelings of insecurity. Therefore, it will be very useful to acquaint your child that all girls and boys will go through the same changes, albeit a little later. The child needs to be reassured that the changes related to his body are normal. Allow him to continue his usual activities (sports, hobby groups). However, some of the benefits of accelerated development may be apparent in these activities. Encourage your child to talk about his or her problems. If you think you need help and advice yourself, consult a child psychologist. A specialist will also advise you; the operation of the school can be a partial help.
Even a preventive early intervention by a psychologist can help increase self-confidence and prevent anxiety in later life.
Parents, relatives and others in the area must choose an appropriate attitude towards the adolescent, his problematic behavior, feelings of guilt and mood swings.
Talking to another child's parents with the same problems can be very helpful. As a rule, the family feels alone and completely unprepared for the premature sexual development of the child. Advice and encouragement from other parents or professionals helps the family to guide and cope with the child's difficulties.
Children with early adolescence may also have difficulty with greater physical strength and height. They get into conflicts with their older siblings and parents. Even in this situation, a child psychologist can help.
Frequently asked questions from parents
How do I explain to my child what premature puberty is?
Explain to your child that the changes taking place in his / her body are now normal and that other children will go through them as well, albeit a little later. If you do not know the advice yourself, ask a child psychologist or specialist for advice.
What should we say to friends, relatives, teachers?
Sometimes parents of children do not want their child to have contact with your child. Therefore, it is essential that you explain the nature of premature adolescence and the difficulties associated with such parents. These people do not realize that your child is completely normal, only a teenager earlier. If your child is being treated with injections, you can also explain the effect of this treatment on the temporary cessation of premature puberty.
Behavioral problems can sometimes persist even with successful treatment. We therefore recommend that you ask for the teacher's cooperation. You can contact your specialist who will help you prepare the letter for school.
What will be your height in adulthood?
Body height depends on many circumstances. In conditions such as premature puberty, it is very difficult to determine probable adult height. The height of the parents and the level of the reached biological age play an important role for the child's height (it can be assessed from the ratio between the child's bone age and the actual or calendar age). Accelerating bone age means that the child has less time to grow. In some cases, bone age may be so significantly accelerated that the final height will be significantly reduced. Some girls with premature puberty may have a very mild form of the disease and may reach virtually normal height depending on their genetic base.
Can treatment help control mental balance?
Generally speaking, the answer is yes. Successful treatment is associated with a decrease in sex hormone levels. However, mood swings are not only affected by hormonal levels, they may also be related to a child's response to changes in his or her physique, self-perception, and experiencing differences from other peers. Relationships with other children and adults can also be significant.
A number of other causes can lead to mood swings and unexpected reactions. Clarifying the reasons is important and it is definitely wise not to link all of your child's difficulties only to his or her premature development.
The parents must explain the difference to the younger child from other children in a way that is proportional to his or her mental maturity. Sometimes this can be done with the help of a fictional story, in which we explain the child's problems in an accessible form and help dispel his worries. Sometimes the help of experts is needed, so the family should contact their specialist if they are not able to cope with the situation.
How long will the treatment last?
Hormone suppression treatment for true premature puberty usually lasts until the child reaches the age suitable for puberty. Generally speaking, treatment is usually stopped around the age of XNUMX, the doctor decides on the basis of bone maturity (corresponds to biological age). Calendar and bone age in a child with premature puberty differ from each other. This means that bone age is accelerated compared to calendar age. After treatment, adolescence resumes and progresses at a normal pace. As already mentioned, in conditions with premature pseudopubertia, the treatment is based on the underlying cause and is different from the treatment of central premature puberty.
Does the treatment have any side effects?
Serious side effects in the treatment of true premature puberty with gonadoliberin analogues are unknown. Very rarely, mild headaches may occur temporarily. Treatment of cyproterone acetate in gonadotropin-independent premature puberty can sometimes be associated with fatigue and feelings of exhaustion, which is associated with a decrease in the production of sex hormones and the hormone cortisol in the adrenal glands.
We need to pay close attention to these children. In case of severe illness or surgery, it may sometimes be necessary to inject Hydrocortisone!
Will our adult child have normal fertility?
Experience shows that the treatment of children with premature puberty with gonadoliberin analogues or cyproterone acetate is not an obstacle to normal fertility. In this sense, long-term studies are carried out, the results of which are evaluated on an ongoing basis.
Constipation
Download full text: Constipation [doc; 44 kB]
Download protocol: Protocol - constipation [doc; 28 kB]
Adequate dietary modification will improve intestinal peristalsis and eliminate laxatives in children treated for constipation. Children's diets must contain sufficient ballast substances. These substances are only contained in foods of plant origin!
Ballast substances swell in the intestine, thus increasing the volume of stool, thus supporting the activity of the intestine (its motility-peristalsis) and thus speeding up the intestinal passage (time required for emptying).
Practical advice:
- Foods that support the digestive process (it is recommended to eat them among the main meals) are yoghurts, kefir, sour milk - the bacteria contained in them have a positive effect on the natural intestinal flora and milk sugar has a laxative effect.
- It is recommended to use milk, fruit sugar: add them to dairy products, muesli, fruit drinks
ATTENTION!!! it has a laxative effect but has the same energy. value as normal sugar - To encourage intestinal motility, it is recommended:
- fast in the morning
- drink one glass of water with 1-2 drops of fruit vinegar
- fresh sauerkraut and a little sauerkraut juice
- use "isolated ballast substances" such as wheat bran mix into yogurt, cottage cheese, muesli, cakes, soups, salads or 3 times a day 1-2 tablespoons of bran drink with water. (Wheat bran softens stool, flax seeds have a similar effect). Because these foods swell in the gut, it is necessary to drink 1 glass of liquid for each teaspoon of bran or seeds.
- Gradually introduce foods rich in ballast into the diet (initial bloating can be alleviated by cumin, fennel and anise)
- Sufficient fluids are a must (2-3 liters of fluids a day), fruit and herbal teas, mineral water, fruit juices without sweetening
- Chew every bite enough and allow enough time for each meal
- Eat fresh vegetables or salad prepared from fresh vegetables at least twice a day
The patient should receive plenty of fruits and vegetables. Fruits and vegetables should be fresh and in the form of oil-fortified salads.
Sauerkraut is especially recommended, which, in addition to the mechanical action of ballast substances, affects the intestine by chemical irritation. Lactic acid acts here, which is also contained in other acidic vegetable supplements and in all acidified dairy products.
From acidic dairy products are recommended: milk butter, yogurt, sour milk, skim milk, kefir and more.
Tartaric, malic and citric acids also help to treat intestinal peristalsis. Intestinal peristalsis is treated even after serving roasted coffee beans and drinks rich in carbonic acid.
Due to its thermal effect, the cold drink, which is served on an empty stomach, also has a beneficial effect on intestinal peristalsis.
The administration of nuts and almonds at a dose of 150-200 g / day has a positive effect. However, these foods are not recommended for obese patients due to their high caloric value.
BALASTIC SUBSTANCES ARE CONTAINED ONLY IN FOODS OF THE VEGETABLE NATURE, THEY ARE RECOMMENDED:
- Cereals and wholegrain products - eg cereal grains - in the form of ground mixtures or flakes (eg as muesli), wholemeal bread, meal, flaxseed bread
- Seeds and kernels: flax, sesame and sunflower seeds, pumpkin kernels - softened during the night, for breakfast with muesli or yoghurt, or mixed with sour milk or kefir
- Fruit:
- Dried fruits - raisins, figs, plums, apricots, dates… (possibly soften in water before use)
- Fresh fruit - all kinds except bananas, especially apples and pears (with peel), raspberries, strawberries, currants, gooseberries
- Nuts, almonds: all kinds, !!! rich in calories, with a tendency not to give overweight
- Vegetables: can be served raw (with oil or cream). Sauerkraut, cauliflower and broccoli are especially recommended
- Legumes: Peas, white and dark beans, lentils
- Potatoes: are preferred over rice and pasta
- Sour dairy products: yogurt, kefir, sour or fatty milk are recommended for their stimulating effect on intestinal peristalsis
FOODS THAT ARE NOT RECOMMENDED BECAUSE THE CONTAINMENT WORKS:
- Confectionery - chocolates, pralines, candies, normal sugar and all the foods in which it is contained
- Bread and pastry - white flour products, desserts, cakes, pastries
- Side dishes - paddy rice, pasta
- Desserts - egg flour products
- Drinks - black tea, cocoa, red wine
- Fruit - only bananas and blueberries
NOTE: The diet must be adjusted according to the age of the child. E.g. fluid intake to adapt to the age of the child, for toddlers and smaller children not to give nuts, etc. !!!
Kidney disorders and transplantation
Download the information brochure Chronic kidney disorders and their transplantation in children and adolescents [in pdf format; 560 kB] for patients' families and for older pediatric patients themselves.
Polycystic kidney disease
in questions and answers for patients' parents
Author Doc.MUDr.Tomáš Seeman, CSc.
Download full text: Polycystic kidney disease in questions and answers for patients' parents [doc; 46 kB]
- What are polycystic kidney diseases?
Polycystic kidney diseases are hereditary diseases affecting the kidneys and manifested by the formation cyst in renal tissue. Cysts are spherical cavities in kidney tissue filled with fluid that is similar in composition to urine. The number of cysts in the kidneys gradually is increasing and so cysts gradually replace healthy kidney tissue and thus impair kidney function.
- What are polycystic kidney diseases?
- How are polycystic kidney diseases inherited?
Polycystic kidney disease is inherited in 2 different hereditary forms:
1) autosomal dominant form (AD, formerly also called "Adult" form of polycystosis)
2) autosomal recessive form (AR, formerly also called "Children's" form).- Autosomal dominant form means that polycystic kidney disease is inherited from generation to generation, regardless of the gender of the individuals (ie from grandmother to father, from father to son) with 50% probability of transmission from an affected parent to a child. This disease is one of the most common hereditary diseases - the incidence in the population is about 1: 1000 people.
- Autosomal recessive form means that polycystic kidney disease affects only one generation, namely 25% of children those two parents who both have one inherited talent for an autosomal recessive form of polycystic kidney disease, both of whom are completely healthy! The reason that 25% of children with polycystic kidney disease can have a completely healthy parent is that they must have two hereditary talents (= 25% of children) for the manifestations of the disease, while only one hereditary talent (= parents) is completely healthy. It occurs significantly less often in the population than the autosomal dominant form, the incidence is approximately 1 affected per 40 people.
These 2 forms with their course and prognosis significantly different, while the so-called "children's" form (autosomal recessive) affects its most severe manifestations almost exclusively children, including infants and newborns, and the so-called "adult" form (autosomal dominant) with its most serious complications manifests itself in adulthood, but even in childhood may manifest some complications that need to be treated and therefore it is appropriate to monitor children with this "adult" form.
- How are polycystic kidney diseases inherited?
- What does polycystic kidney disease affect?
Autosomal recessive (AR) form polycystosis of the kidneys is manifested mainly by symptoms of kidney damage such as:- small multiple cysts in the kidneys
- enlargement of the kidneys (sometimes up to extreme dimensions, when enlarged kidneys fill practically the entire abdominal cavity and arching significantly the abdomen)
- urinary tract infections, including kidney inflammation
- protein in urine
- blood in urine
- increased blood pressure (blood pressure often reaches extreme values that can damage the heart and blood vessels)
- development of chronic renal failure with the need for dialysis and transplantation (the most serious symptom of the disease !, it occurs in 20-50% of patients as children).
Some children even they die just after childbirth or in early infancy, with the most common cause of death being congenital lung damage.
Another manifestation of the autosomal recessive form of polycystic kidney disease iscongenital liver fibrosis (= replacement of liver tissue with connective tissue), which leads to worsening of blood flow to the liver with consequent enlargement of the spleen.
As can be seen, the autosomal recessive form of polycystosis of the kidneys is a disease that affects not only the kidneys but affects multiple organs of the whole body.
Autosomal dominant (AD, older name "adult") formpolycystosis of the kidneys, as the name "adult" suggests, begins to manifest itself in subjective difficulties (back pain, abdominal pain, headache, urinary tract infections, kidney colic with kidney stones) mostly in adulthood, but most individuals have symptoms of the disease as early as childhood, although they do not usually cause these symptoms in childhood no subjective difficulties. These manifestations include:- larger multiple cysts in the kidneys
- kidney enlargement (mostly small or medium scale)
- urinary tract infections, renal cysts, renal inflammation
- protein in urine
- blood in urine
- increased blood pressure (blood pressure is usually only slightly increased, but it can also damage the heart and blood vessels in children)
- development of chronic renal failure (again, the most serious symptom of the disease, which, however, occurs very rarely in children and usually affects adults up to 50-60 years of age on average).
Like the "childish" form, the "adult" form - an autosomal dominant form of polycystic kidney disease - is a disease that affects not only the kidneys but more organs and especially:- liver, spleen, pancreas, ovaries (cysts may appear in all organs)
- heart (heart valve defects, consequences of increased blood pressure)
- cerebral arteries (bulging = aneurysms).
- What does polycystic kidney disease affect?
- How can polycystic kidney disease be detected?
The best method to detect kidney polycystosis is to find them ultrasound = sonography = ultrasonography. Ultrasound examination very reliably detects the presence of cysts in the kidney tissue. However, cysts do not have to be sonographically detectable in AD - the "adult form" in early childhood, so the sonographic examination must often be repeated.
If there is at least 1 person with polycystic kidney disease in the family (preferably 2 or more patients), it is possible to perform molecular genetic testing, for which it is necessary to take blood from all family members, even from healthy individuals. The result of this molecular genetic examination can, under certain conditions, tell us s 99-100% probability, whether or not the individual has inherited a talent (affected gene) for polycystosis and will therefore develop the disease at a certain age. Autosomal dominant polycystosis of the kidneys is caused by mutations in 2 genes. Patients with mutations in the second gene have a better long-term prognosis than patients with mutations in the first gene, so molecular genetic testing is important not only in making the diagnosis (determining whether or not the patient has polycystic kidney disease) but also prognostic. Autosomal recessive polycystosis of the kidneys is caused by mutations in a single gene; molecular genetic testing of this gene has not yet been performed in the Czech Republic.
At present, it is possible as well prenatal diagnosis (examination before the birth of a child) molecular genetic examination, which means that it is possiblealready during pregnancy (prenatally) with 99-100% confidence to say if the fetus is affected polycystic kidney disease and in case of a positive finding and the family's wishes, this pregnancy can be artificially terminated and thus prevent the birth of an individual affected by this serious disease.
- How can polycystic kidney disease be detected?
- Polycystic kidney diseases can be treated, resp. heal?
Because polycystic kidney disease is caused by damage to the genetic - hereditary equipment of an individual, which we have not yet been able to "fix", therefore, they cannot be cured (ie to prevent the development of the disease), however, its manifestations and complications such as urinary tract infections, high blood pressure, proteinuria and especially chronic kidney failure can be treated. Chronic renal failure is the most serious manifestation of the disease and is treated in its final stages by dialysis ("artificial kidney") and kidney transplantation.
Early detection of these treatable manifestations and complications of the disease and their timely and consistent treatment can alleviate the course of polycystic kidney disease and thus improve the long-term adverse prognosis of patients with this disease. Therefore, regular check-ups in the children's nephrology clinic are very important (= kidney disease clinic), which focus on early detection of the symptoms and their treatment.
Our Department of Pediatrics (formerly I. Children), University Hospital in Prague - Motol deals with the follow-up of patients with both forms of polycystic kidney disease. He currently works with many pediatric nephrologists from all over the Czech Republic in follow-up of over 200 children with polycystic kidney disease a provides for these pediatric patients complete medical services from the nephrology clinic through the inpatient nephrology department, genetic and ultrasound examinations to the dialysis and transplantation program for those children who develop chronic kidney failure.
Further information for patients and parents of patients with polycystic kidney disease is available in English on the websites of various nephrological societies, such as:
- https://www.pkdcure.org
- https://kidney.niddk.nih.gov/kudiseases/pubs/polycystic/
- https://www.kidney.org/atoz/atozItem.cfm?id=102
Prague, May 2007
Doc.MUDr.Tomáš Seeman, CSc.
Department of Pediatrics, Motol University Hospital
V Úvalu 84, 150 06 Prague 5
tel .: 2 / 2443-2034
fax: 2 / 2443-2020
Email: tomas.seeman@lfmotol.cuni.cz
Seminars
Regional seminars
The Pediatric Clinic regularly organizes seminars for primary departments of children's wards and their collaborators. Doctors present interesting case reports, recommended procedures and new trends in treatment.
The directory of regular participants in "primary seminars" has so far been limited mainly to the Central Bohemian Region and Prague. If you are not in the directory as the primary department of the children's ward and you are interested in regular participation, we will be happy to welcome you. Please inform Secretary Bendová (e-mail: helena.bendova@lfmotol.cuni.cz).
The main goal of the Pediatric Clinic of the 2nd Faculty of Medicine of Charles University and the University Hospital in Motol is to provide highly specialized and erudite care to children from all over the Czech Republic.
In almost all areas of pediatrics and adolescent medicine, the Pediatric Clinic has highly qualified specialists - in pediatric nephrology, dialysis and elimination methods, pediatric pneumology, allergology and care for children with cystic fibrosis, pediatric endocrinology and diabetology, pediatric gastroenterology and care. about children with autoimmune diseases. In cooperation with partner workplaces of the Motol University Hospital, we also provide cardiological, immunological and hematological care.
We are ready to help you and your patients whenever you deem it necessary.
Medical seminars of the Pediatric Clinic
Medical seminars of the Pediatric Clinic are held from September to June every Monday, Wednesday and Friday from 7.45 am to 8.30 am in Brdlík's seminar room, entrance through the building of the children's part of the hospital, 1st floor, node D - secretariat. Guests from other workplaces are welcome.
Attendance is recommended for final year students of medical studies.
The current seminar program will be sent to you upon request by the clinic secretary Helena Bendová (helena.bendova@lfmotol.cuni.cz).
Research
List of publications
The list of publications of the staff of the Pediatric Clinic in individual years can be found at https://www.lf2.cuni.cz/info2lf/ustavy/2dk/publik.htm.
Graduate students
MD Katarína Beránková - Early manifestations of bronchial asthma in childhood. Morphological and functional origins of the disease
Field council: Human physiology and pathophysiology
Supervisor: Prof. MUDr. Petr Pohunek, CSc.
MD Jana Djakow - Aspects of identification of patients with primary ciliary dyskinesia
Field council: Human physiology and pathophysiology.
Supervisor: MUDr. Ondřej Cinek, Ph.D., supervisor consultant: Prof. MUDr. Petr Pohunek, CSc.
MD Katarína Mitrová - New regulatory hormones of breast milk
Field board: Biochemistry and pathobiochemistry
Supervisor: MUDr. Jiří Bronský, Ph.D.
MD Lenka Petruželková - Study of first-degree relatives from families of patients with type 1 diabetes mellitus
Field council: Human physiology and pathophysiology
Supervisor: Prof. MUDr. Jan Lebl, CSc., Supervisor consultant: Doc. MUDr. Katerina Stechova, Ph.D.
MD Tereza Ulmannová - Altered gene expression after specific stimulation in first-degree patients with T1D
Field Council: Molecular and Cellular Biology, Genetics and Virology
Supervisor: Doc. MUDr. Katerina Stechova, Ph.D.
M.Sc. Šárka Vošahlíková - Gram-negative pathogens in patients with cystic fibrosis.
Field Council: Molecular and Cellular Biology, Genetics and Virology.
Supervisor: MUDr. Ondrej Cinek, Ph.D.
MD Tomáš Dědic - The role of hereditary factors in the etiology and pathogenesis of childhood cholestatic diseases
Field council: Human physiology and pathophysiology
Supervisor: MUDr. Radana Kotalova, CSc.
Havlišová Magdaléna, MD - Occurrence and importance of secondary ciliary dyskinesia in various types of resorption diseases
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Petr Pohunek, CSc .; MUDr. Jiří Uhlík, Ph.D.
MD Lenka Hoňková - Mechanisms and features of airway wall remodeling in bronchial asthma and other chronic respiratory diseases and their relationship to the course of the disease and changes in respiratory physiology
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Petr Pohunek, CSc.
MD Lucia Karnišová - Hemolytic-uremic syndrome: etiology, genetic profile of patients, identification of other possible pathogenetic factors of the disease
Field council: Human physiology and pathophysiology
Supervisor: doc. MUDr. Kveta Blahova, CSc.
MUDr. Vaclav Koucky - Detection of early changes in lung function in infants and young children with cystic fibrosis, asthma risk and other respiratory diseases
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Petr Pohunek, CSc.
Sage. Lenka Kramná - Picornaviruses in the pathogenesis of islet autoimmunity
Field council: Molecular and cell biology, genetics
Supervisor: Doc. MUDr. Ondrej Cinek, Ph.D.
M.Sc. Jana Matasková - Use of mechanography in the diagnosis of muscle damage in children with chronic diseases
Field council: Human physiology and pathophysiology
Supervisor: doc. MUDr. Zdenek Sumnik, Ph.D.
MD Jan Ohem - Optimization of biological treatment of nonspecific intestinal inflammation (IBD) in children using modern biomarkers
Field board: biochemistry and pathobiochemistry
Supervisor: doc. MUDr. Jiří Bronský, Ph.D.
M.Sc. MD Tomáš Rosík - Proteinuria and its relation to the survival of transplanted kidneys in children
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Tomas Seeman, CSc.
MD Klára Roženková - Influence of mutations in selected genes on beta cell function
Field council: Human physiology and pathophysiology
Supervisor: doc. MUDr. Štěpánka Průhová, Ph.D.
MUDr. Vojtech Sedivy - Influence of perinatal insults on the development of pulmonary vascular circulation
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Jan Herget, DrSc., Prof. MUDr. Vaclav Chaloupecky, CSc.
MD Nadežda Šimánková - BKV polyomavirus in children after kidney transplantation
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Tomas Seeman, CSc.
MUDr. Pera Simunkova - Morphometric and immunohistochemical evaluation of airway wall remodeling in experimentally induced bronchial asthma
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Petr Pohunek, CSc., MD Jiří Uhlík, Ph.D.
M.Sc. Jana Včeláková - Polarization in the direction of Th17 in people really at risk of developing type 1 diabetes
Field council: Immunology
Supervisor: doc. MUDr. Katerina Stechova, Ph.D.
Labs
Laboratory of Molecular Genetics - www.lmg.cz
Laboratory of Autoimmune Diseases - www.labao.cz
Regional seminars
The Pediatric Clinic regularly organizes seminars for primary departments of children's wards and their collaborators. Doctors present interesting case reports, recommended procedures and new trends in treatment.
The directory of regular participants in "primary seminars" has so far been limited mainly to the Central Bohemian Region and Prague. If you are not in the directory as the primary department of the children's ward and you are interested in regular participation, we will be happy to welcome you. Please inform Secretary Bendová (e-mail: helena.bendova@lfmotol.cuni.cz).
The main goal of the Pediatric Clinic of the 2nd Faculty of Medicine of Charles University and the University Hospital in Motol is to provide highly specialized and erudite care to children from all over the Czech Republic.
In almost all areas of pediatrics and adolescent medicine, the Pediatric Clinic has highly qualified specialists - in pediatric nephrology, dialysis and elimination methods, pediatric pneumology, allergology and care for children with cystic fibrosis, pediatric endocrinology and diabetology, pediatric gastroenterology and care. about children with autoimmune diseases. In cooperation with partner workplaces of the Motol University Hospital, we also provide cardiological, immunological and hematological care.
We are ready to help you and your patients whenever you deem it necessary.
Medical seminars of the Pediatric Clinic
Medical seminars of the Pediatric Clinic are held from September to June every Monday, Wednesday and Friday from 7.45 am to 8.30 am in Brdlík's seminar room, entrance through the building of the children's part of the hospital, 1st floor, node D - secretariat. Guests from other workplaces are welcome.
Attendance is recommended for final year students of medical studies.
The current seminar program will be sent to you upon request by the clinic secretary Helena Bendová (helena.bendova@lfmotol.cuni.cz).
List of publications
The list of publications of the staff of the Pediatric Clinic in individual years can be found at http://www.lf2.cuni.cz/info2lf/ustavy/2dk/publik.htm
Postgraduate
and students
MD Katarína Beránková - Early manifestations of bronchial asthma in childhood. Morphological and functional origins of the disease
Field council: Human physiology and pathophysiology
Supervisor: Prof. MUDr. Petr Pohunek, CSc.
MD Jana Djakow - Aspects of identification of patients with primary ciliary dyskinesia
Field council: Human physiology and pathophysiology.
Supervisor: MUDr. Ondřej Cinek, Ph.D., supervisor consultant: Prof. MUDr. Petr Pohunek, CSc.
MD Katarína Mitrová - New regulatory hormones of breast milk
Field board: Biochemistry and pathobiochemistry
Supervisor: MUDr. Jiří Bronský, Ph.D.
MD Lenka Petruželková - Study of first-degree relatives from families of patients with type 1 diabetes mellitus
Field council: Human physiology and pathophysiology
Supervisor: Prof. MUDr. Jan Lebl, CSc., Supervisor consultant: Doc. MUDr. Katerina Stechova, Ph.D.
MD Tereza Ulmannová - Altered gene expression after specific stimulation in first-degree patients with T1D
Field Council: Molecular and Cellular Biology, Genetics and Virology
Supervisor: Doc. MUDr. Katerina Stechova, Ph.D.
M.Sc. Šárka Vošahlíková - Gram-negative pathogens in patients with cystic fibrosis.
Field Council: Molecular and Cellular Biology, Genetics and Virology.
Supervisor: MUDr. Ondrej Cinek, Ph.D.
MD Tomáš Dědic - The role of hereditary factors in the etiology and pathogenesis of childhood cholestatic diseases
Field council: Human physiology and pathophysiology
Supervisor: MUDr. Radana Kotalova, CSc.
Havlišová Magdaléna, MD - Occurrence and importance of secondary ciliary dyskinesia in various types of resorption diseases
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Petr Pohunek, CSc .; MUDr. Jiří Uhlík, Ph.D.
MD Lenka Hoňková - Mechanisms and features of airway wall remodeling in bronchial asthma and other chronic respiratory diseases and their relationship to the course of the disease and changes in respiratory physiology
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Petr Pohunek, CSc.
MD Lucia Karnišová - Hemolytic-uremic syndrome: etiology, genetic profile of patients, identification of other possible pathogenetic factors of the disease
Field council: Human physiology and pathophysiology
Supervisor: doc. MUDr. Kveta Blahova, CSc.
MUDr. Vaclav Koucky - Detection of early changes in lung function in infants and young children with cystic fibrosis, asthma risk and other respiratory diseases
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Petr Pohunek, CSc.
Sage. Lenka Kramná - Picornaviruses in the pathogenesis of islet autoimmunity
Field council: Molecular and cell biology, genetics
Supervisor: Doc. MUDr. Ondrej Cinek, Ph.D.
M.Sc. Jana Matasková - Use of mechanography in the diagnosis of muscle damage in children with chronic diseases
Field council: Human physiology and pathophysiology
Supervisor: doc. MUDr. Zdenek Sumnik, Ph.D.
MD Jan Ohem - Optimization of biological treatment of nonspecific intestinal inflammation (IBD) in children using modern biomarkers
Field board: biochemistry and pathobiochemistry
Supervisor: doc. MUDr. Jiří Bronský, Ph.D.
M.Sc. MD Tomáš Rosík - Proteinuria and its relation to the survival of transplanted kidneys in children
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Tomas Seeman, CSc.
MD Klára Roženková - Influence of mutations in selected genes on beta cell function
Field council: Human physiology and pathophysiology
Supervisor: doc. MUDr. Štěpánka Průhová, Ph.D.
MUDr. Vojtech Sedivy - Influence of perinatal insults on the development of pulmonary vascular circulation
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Jan Herget, DrSc., Prof. MUDr. Vaclav Chaloupecky, CSc.
MD Nadežda Šimánková - BKV polyomavirus in children after kidney transplantation
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Tomas Seeman, CSc.
MUDr. Pera Simunkova - Morphometric and immunohistochemical evaluation of airway wall remodeling in experimentally induced bronchial asthma
Field council: Human physiology and pathophysiology
Supervisor: prof. MUDr. Petr Pohunek, CSc., MD Jiří Uhlík, Ph.D.
M.Sc. Jana Včeláková - Polarization in the direction of Th17 in people really at risk of developing type 1 diabetes
Field council: Immunology
Supervisor: doc. MUDr. Katerina Stechova, Ph.D.
Labs
Laboratory of Molecular Genetics
www.lmg.cz
Laboratory of autoimmune diseases
www.labao.cz
Specialization
Dear friends, colleagues, co-workers and sponsors, pediatric patients and their parents!
The Department of Pediatrics of the 2nd Faculty of Medicine of Charles University and the University Hospital in Motol was established in 2004 by merging the work teams of the former I. children's clinic and a significant part of the former II. children's clinic. It is a continuation of their mission - to provide highly specialized and erudite care to children from all over the Czech Republic, whose doctors or parents have requested it. The team of the Pediatric Clinic creates a natural professional background, the "ultimum refugium", for all Czech and Moravian pediatricians, whether they work in children's clinics of teaching hospitals, district children's wards or work as general practitioners for children and adolescents. We are ready to help you and your patients whenever you deem it necessary.
You also meet the staff of the Pediatric Clinic in undergraduate and postgraduate education in pediatrics and its subspecializations, in organizational activities in the care of sick children at the national level and in clinical research and development of biomedical knowledge for the benefit of pediatric patients.
In almost all areas of pediatrics and adolescent medicine, the Pediatric Clinic has highly qualified specialists who provide top diagnostics and therapy - in pediatric nephrology, dialysis and elimination methods, pediatric pneumology and care for children with cystic fibrosis, pediatric endocrinology and diabetology, in pediatric gastroenterology and in the care of children with autoimmune diseases. In cooperation with partner workplaces of the Motol University Hospital, we also provide cardiological, immunological and hematological care.
The credo of the Pediatric Clinic team is "partnership for the benefit of pediatric patients". We are here for you and your patients. Our strength lies in the team experience, in the quality equipment and in the cooperation of the pediatric think tank of the Motol hospital. We strive for straightforward, fast and effective diagnosis and therapy with maximum care for our common pediatric patients.
Our work would be more difficult without sponsors, who make a significant contribution to the renewal and expansion of the clinic's equipment, our "instruments", but also to a friendly and aesthetic environment for our patients. Many thanks to all our sponsors, the clinic team and our patients.
Thanks also go to all Czech and Moravian pediatricians in primary care and inpatient facilities. We highly value their daily endless efforts. It is thanks to them and their work that the sick children who need it most come to us. We thank them for recommending and sending these patients to us. I am sure that it is through our joint efforts that we achieve the maximum possible for the well-being of sick children.
Prof. MD Jan Lebl, CSc.,
on behalf of the team of doctors and nurses of the Pediatric Clinic
Contact
Address:
V Úvalu 84
150 06, Prague 5
Knowledge:
head - Prof. MUDr. Zdenek Sumnik, Ph.D.
Chief Medical Officer – primary doc. MD Štěpánka Průhová, Ph.D.
head nurse - Mgr. Jana Boháčová, phone: +420 22443 2005
Secretariat:
Medical Secretariat
Jana Šašková, phone: +420 22443 2002
Lenka Viktorinová, phone: +420 22443 2004
School secretariat
Klára Borecká, phone: +420 22443 2001
fax: + 420 22443 2020
Email: pediatrie@fnmotol.cz, pediatrie@lfmotol.cuni.cz
Contact with health insurance companies
Jitka Doubravová
phone: 224 432 007
Email: jitka.doubravova@fnmotol.cz
Workplace
| cardiology outpatient clinic - ECG | 6th floor Polyclinic | 224 432 073 |
| nephrology clinic | S1. floor B - bed part | 224 432 080, 2086 |
| diabetological outpatient clinic | 1th floor Polyclinic | 224 433 813, 3811 |
| endocrinology clinic | 1th floor Polyclinic | 224 433 813, 3811 |
| gastroenterological outpatient clinic | 1th floor Polyclinic | 224 432 031, 2013 |
| anthropology | 1th floor Polyclinic | 224 432 260 |
| pneumological outpatient clinic | 1th floor Polyclinic | 224 432 012 |
| cystic fibrosis center | SP. floor Polyclinic | 224 432 227, 2230 |
| examination of chlorides in sweat | 1th floor Polyclinic | 224 432 272, 2067 |
| spirometry | 1th floor Polyclinic | 224 432 265, 2067 |
| obesitology | 1th floor Polyclinic | 224 433 821 |
| pediatrics | 1th floor Polyclinic | 224 432 042, 2044, 3812 |
| pediatrics - nurse | 1th floor Polyclinic | 224 433 816 |
| comprehensive care center | 1th floor Polyclinic | 224 433 790 |
| gastroenterology department | P. floor A - bed part | 224 432 011, 2039 |
| infant ward | P. floor C - bed part | 224 432 033 |
| nephrology department | 1st floor C - bed part | 224 432 234, 2240 |
| Department of Diabetology and Endocrinology | 1st floor B - bed part | 224 432 010, 2029 |
| Department of Pneumology and Allergology | 1st floor A - bed part | 224 432 207, 2032 |
| Intensive Care Unit | P. floor B - bed part | 224 432 238, 2278, 2208 |
The Pediatric Clinic is located on the premises of the University Hospital in Motol, in a children's monoblock - department PC, 1C, PA, 1A, S1B, -1C
Transport connection:
- from metro line A - Motol Hospital station
- from metro line A - station Dejvická by bus number 180
- from metro line A - Hradčanská station by bus number 184
- from metro line B - station Anděl by bus number 167
- from metro line B - Nové Butovice station by buses number 179 or 168
- from Hlavní nádraží by tram number 9 direction Anděl and at Anděl change to bus no. 167
- night bus number 502
In all these cases, it is an exit station Motol Hospital.
Examination orders
To order, you must have a written recommendation from a district doctor or specialist.
You can order at the contacts below, prefer e-mail communication.
| cardiology outpatient clinic - ECG | 224 432 073 |
| nephrology clinic | 224 432 080, 2086 |
| diabetological outpatient clinic | 224 433 813, 3811 |
| endocrinology clinic | 224 433 813, 3811 |
| gastroenterological outpatient clinic | 224 432 031, 2013 gastroped@fnmotol.cz |
| anthropology | 224 432 260 |
| pneumological outpatient clinic | 224 432 012 pneumoamb@fnmtol.cz |
| cystic fibrosis center | 224 432 227 cfdeti@fnmotol.cz |
| examination of chlorides in sweat | 224 432 272 |
| spirometry | 224 432 265 |
| gastroenterology department | 224 432 011 |
| infant ward | 224 432 033 kojenci@fnmotol.cz |
| nephrology department | 224 432 240, 2234 |
| Department of Diabetology and Endocrinology | 224 432 010, 2029 |
| pneumology department | 224 432 207, 2032 |
| obesitology | 224 433 821 obezitologiedeti@fnmotol.cz |
| general pediatrics - nurse | 224 433 816 |